NEJM:里程碑式研究:弥漫性大B细胞淋巴瘤分类迈出更精准一步
2018-04-16 王强 肿瘤资讯
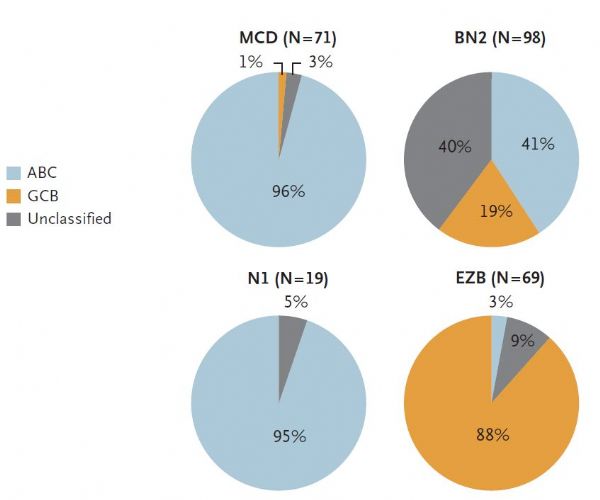
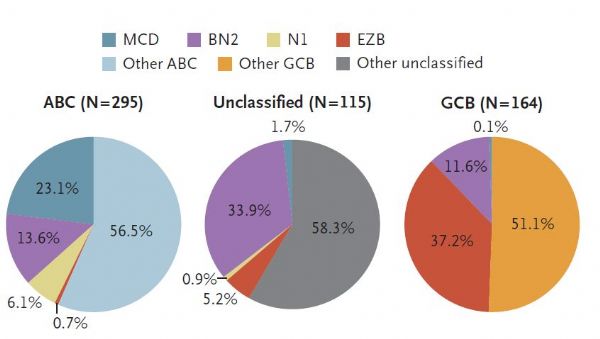
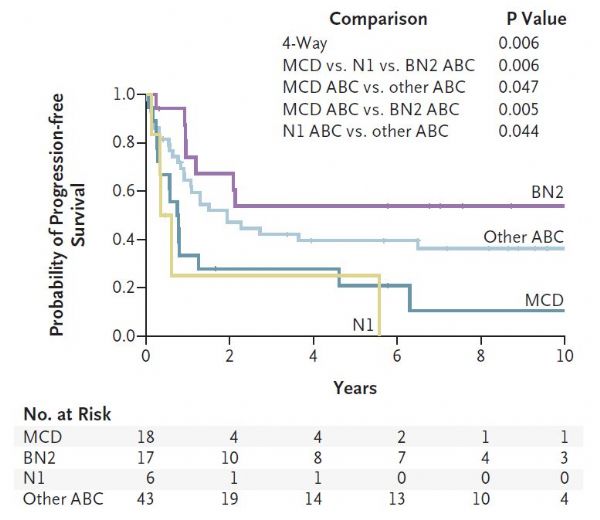
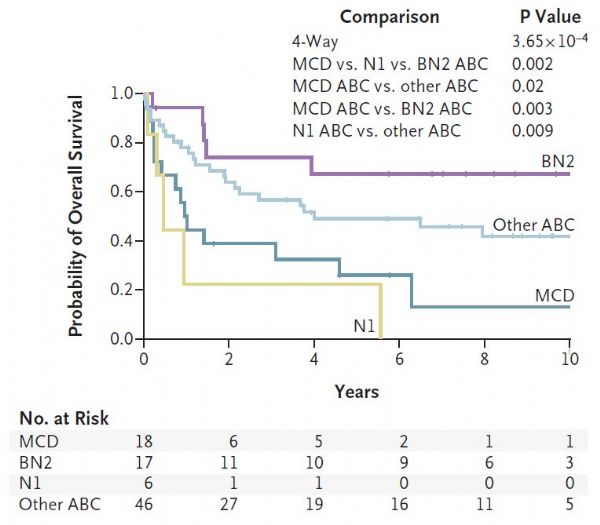
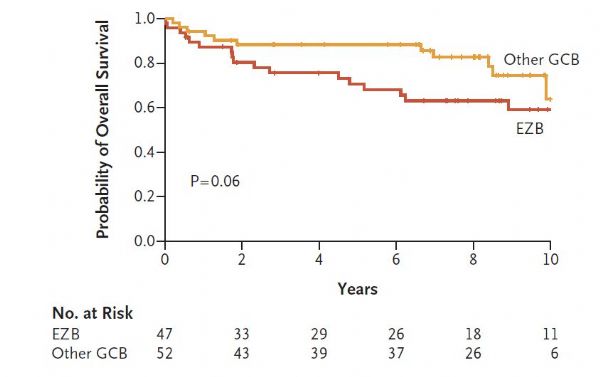
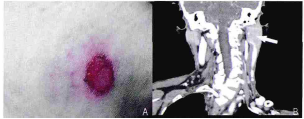
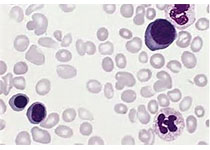
弥漫性大B细胞淋巴瘤是最常见的淋巴瘤类型,按照世界卫生组织分类可以分为三种类型,但即使同一类型中的患者也会有疗效及预后的差异。最近发表于《新英格兰医学杂志》上的一项研究对该肿瘤进行了进一步的遗传学分类,被专业人士评为 “里程碑”式的研究。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#里程碑#
43
#细胞淋巴瘤#
40
#里程碑式研究#
62
#B细胞#
48
#弥漫性大B细胞淋巴瘤#
48
#精准#
38
#弥漫性#
41