Cell Metab:肥胖为何诱发糖尿病?科学家找到重要“推手”
2016-04-08 佚名 生物谷
本文亮点: 高脂饮食会增加附睾旁脂肪组织内的NK细胞数目并促进NK细胞激活 附睾旁脂肪组织内的NK细胞能够调节肥胖模型中脂肪组织巨噬细胞介导的炎症 脂肪组织内的NK细胞能够调节肥胖诱导的胰岛素抵抗进展 最近,来自哈佛大学医学院的研究人员在国际学术期刊cell metabolism上发表了一项最新研究进展,他们发现附睾旁脂肪组织内的自然杀伤细胞(NK细胞)能够通过影响脂肪组织巨噬细胞介
本文亮点:
高脂饮食会增加附睾旁脂肪组织内的NK细胞数目并促进NK细胞激活
附睾旁脂肪组织内的NK细胞能够调节肥胖模型中脂肪组织巨噬细胞介导的炎症
脂肪组织内的NK细胞能够调节肥胖诱导的胰岛素抵抗进展

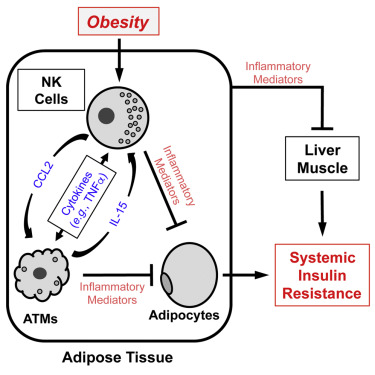
最近,来自哈佛大学医学院的研究人员在国际学术期刊cell metabolism上发表了一项最新研究进展,他们发现附睾旁脂肪组织内的自然杀伤细胞(NK细胞)能够通过影响脂肪组织巨噬细胞介导的炎症促进肥胖诱导的胰岛素抵抗进展。这对于肥胖及肥胖相关代谢综合征(2型糖尿病等)的机制研究以及治疗方法开发具有重要意义。
许多研究证明在肥胖小鼠模型中,脂肪组织内的免疫细胞介导的炎症会参与胰岛素抵抗的发生,特别是以附睾旁脂肪组织为代表的内脏脂肪,对于系统性胰岛素抵抗的贡献非常显著,而脂肪组织内驻留的巨噬细胞是诱导脂肪组织炎症的重要免疫细胞类型,但除巨噬细胞之外的其他免疫细胞是否也参与脂肪组织炎症的进展目前仍然没有得到很好的研究。
在这项最新研究中,研究人员发现脂肪组织内的自然杀伤细胞(NK细胞)在肥胖诱导的胰岛素抵抗过程中也发挥重要作用。他们发现高脂饮食能够增加脂肪组织内的NK细胞数目,同时包含TNFa在内的一系列促炎症因子的合成也出现增加,但这一现象只发现于附睾旁脂肪组织,在皮下脂肪组织中并没有观察到这一现象。
研究人员通过中和抗体以及E4bp4+/-小鼠清除NK细胞,结果发现肥胖诱导的胰岛素抵抗得到改善,同时伴有脂肪组织巨噬细胞数目减少以及脂肪组织巨噬细胞介导的炎症水平下降。与之相比,给予IL-15处理或将NK细胞导入E4bp4-/-小鼠来增加NK细胞的数目既会增加脂肪组织巨噬细胞的数目和脂肪组织的炎症水平,还会加速高脂饮食诱导的胰岛素抵抗进展。
这些结果表明脂肪组织中的NK细胞能够在脂肪组织巨噬细胞的上游通过产生TNFa等促炎症因子控制脂肪组织巨噬细胞的行为,进而促进肥胖诱导的胰岛素抵抗的进展。这项研究为深入理解免疫系统与胰岛素抵抗之间的关系提供了重要信息。
原始出处:
Byung-Cheol Lee,et al.Adipose Natural Killer Cells Regulate Adipose Tissue Macrophages to Promote Insulin Resistance in Obesity.Cell metabolism.DOI: http://dx.doi.org/10.1016/j.cmet.2016.03.002.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Meta#
65
#MET#
56
#Cell#
65
#CEL#
59
文章值得关注
142
??………………
126
为什么是附睾
176