Nat Commun:一种诊断且治疗肺癌的新方法
2016-07-14 佚名 生物谷
近日,一项刊登于国际杂志Nature Communications上的研究报告中,来自新加坡的研究人员通过研究发现了一类名为oncomiRs的小RNA分子,其是引发肺癌发生的主要原因,相关研究或为理解肺癌对疗法产生耐药性的机制,以及有效监测并且开发治疗肺癌的新型疗法提供思路。文章中,研究者揭示了,肿瘤内罕见的癌症干细胞对常规疗法会产生耐受性,这就常常会引发肺癌患者疾病复发,由于oncomiRs分子
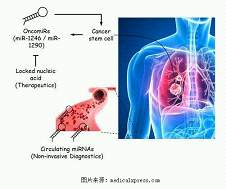
近日,一项刊登于国际杂志Nature Communications上的研究报告中,来自新加坡的研究人员通过研究发现了一类名为oncomiRs的小RNA分子,其是引发肺癌发生的主要原因,相关研究或为理解肺癌对疗法产生耐药性的机制,以及有效监测并且开发治疗肺癌的新型疗法提供思路。
文章中,研究者揭示了,肿瘤内罕见的癌症干细胞对常规疗法会产生耐受性,这就常常会引发肺癌患者疾病复发,由于oncomiRs分子是癌症干细胞的主要驱动子,因此剔除oncomiRs分子的新型疗法或许可以帮助我们杀灭癌症干细胞,为此研究人员利用了一系列名为锁核酸(locked nucleic acid,LNA)的治疗方法,该方法可以抵御癌症干细胞中的oncomiRs分子,研究者表示,这种方法可以成功阻断小鼠模型中人类肺部肿瘤的生长,如今研究者们正在同制药公司联合开发一种可以直接用于人类机体的新型药物。
研究人员表示,通过对患者的液体活检标本进行检测就能够发现oncomiRs分子,液体活检技术是一种相对于组织活检而言侵入性较低消耗时间较短的技术,实际上oncomiRs分子可以帮助指示是否患者会对常规疗法产生反应或者屈服于疾病;因此实时追踪接受标准化疗法患者血液中的oncomiRs分子的水平或许可以帮助科学家监测患者机体的反应以及潜在预测患者疾病的复发及癌症转移情况。
研究者Tam博士表示,将这种检测方法开发成为一种伴随诊断技术或可改善对疾病的追踪情况,并且可以为我们提供肿瘤进展的实时信息;此外我们还希望能够通过理解驱动肺癌的关键驱动子来克服肿瘤对疗法产生耐药性等问题,以便后期我们能够开发出新型方法来改善病人对疗法应答的持久性以及健康状况。
最后研究者表示,靶向做作用肿瘤中“最顽强”的细胞可以帮助我们直接攻击引发癌症的根源性问题,这对于理解癌症进展非常重要;同时本文研究也为后期科学家和肿瘤学家改善对病人的分层以及开发新型精准性靶向疗法提供新的思路和希望。
原始出处
Wen Cai Zhang, Tan Min Chin, Henry Yang, Min En Nga, Declan Patrick Lunny, Edwin Kok Hao Lim, Li Li Sun, Yin Huei Pang, Yi Ning Leow, Shanneen Rossellini Y Malusay, Priscilla Xin Hui Lim, Jeravan Zili Lee, Benedict Jian Wei Tan, Ng Shyh-Chang, Elaine Hsuen Lim, Wan Teck Lim, Daniel Shao Weng Tan, Eng Huat Tan, Bee Choo Tai, Ross Andrew Soo et al.Tumour-initiating cell-specific miR-1246 and miR-1290 expression converge to promote non-small cell lung cancer progression.Nat Commun.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Nat#
76
#新方法#
58
#COMMUN#
64
不错哦继续关注
105
值得关注
179
好文章
115
学习了很多的方法
158
学习啦!
132