Cell:维生素C可能促使血癌干细胞死亡,有望抗白血病
2017-08-18 佚名 medicalxpress
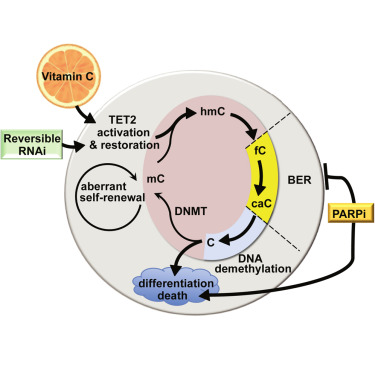
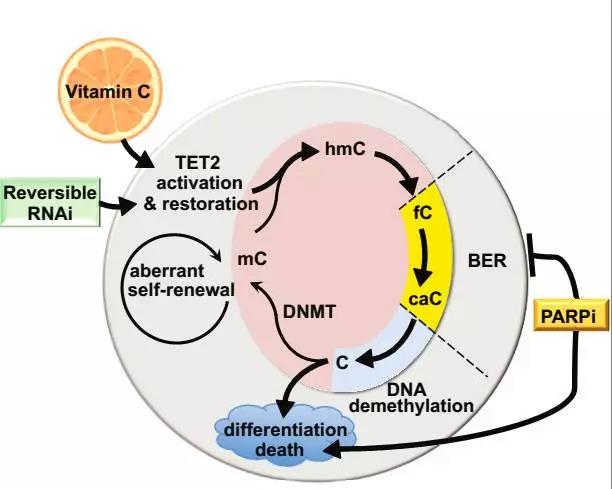
维生素C可以“告知”骨髓中的有缺陷的干细胞成熟并正常死亡,而不是倍增引起血液癌。这是由纽约大学Langone Health Perlmutter癌症中心的研究人员领导的一项研究的发现,并于8月17日在“Cell”杂志上发表。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
0
#Cell#
63
总量有参考吗?
131
学习
92
#癌干细胞#
81
#血癌#
80
很好的文章,学习了
96
很好,不错,以后会多学习
146