Cell:免疫疗法大牛James Allison全新:PD-1抗体与CTLA-4抗体原来如此不同
2017-08-14 佚名 生物探索
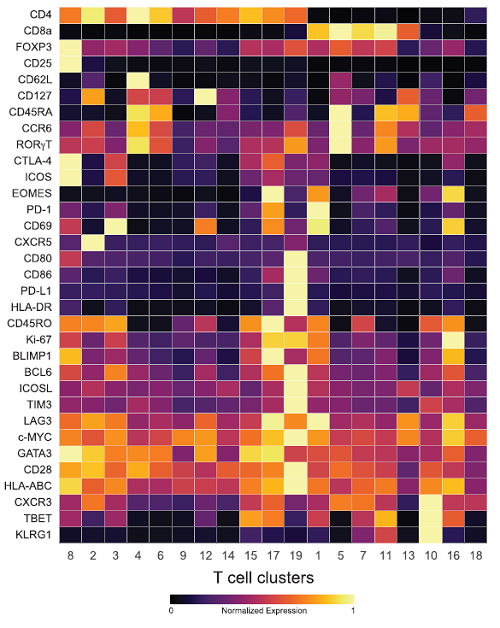
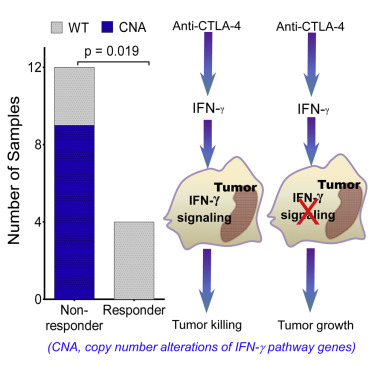
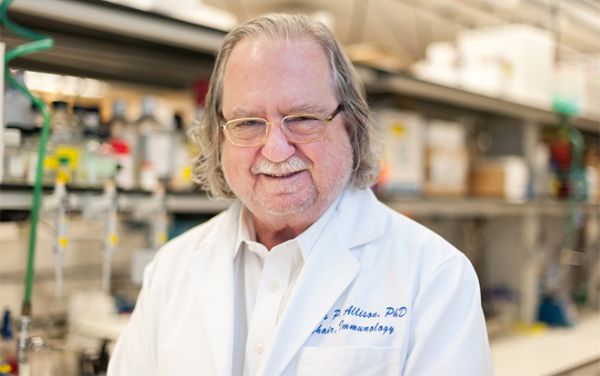
MD安德森癌症中心的James P. Allison教授是癌症免疫疗法的先驱之一,也被称“CTLA-4抗体Yervoy之父”。去年,他还荣获了有着诺奖风向标之称的汤森路透“引文桂冠奖”。近日,他带领的研究小组在Cell杂志上发表了一项新成果,揭开了CTLA-4抗体和PD-1抗体这两类癌症免疫疗法不同的细胞机制。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Cell#
47
#CEL#
53
#ALL#
68
#CTLA-4#
61
#PD-1抗体#
61
#MES#
69