J Periodontal Res:精神障碍患者的牙周炎发病率较高
2020-12-07 MedSci原创 MedSci原创
常见精神障碍的特点是存在烦躁、疲劳、失眠、健忘、专注力下降、焦虑和抑郁。精神障碍与多种疾病有关,但很少有研究将其与牙周炎联系起来。一项横断面研究评估了暴露于常见精神障碍(CMD)与牙周炎之间的关联,研
常见精神障碍的特点是存在烦躁、疲劳、失眠、健忘、专注力下降、焦虑和抑郁。精神障碍与多种疾病有关,但很少有研究将其与牙周炎联系起来。一项横断面研究评估了暴露于常见精神障碍(CMD)与牙周炎之间的关联,研究结果已在线发表于J Periodontal Res。

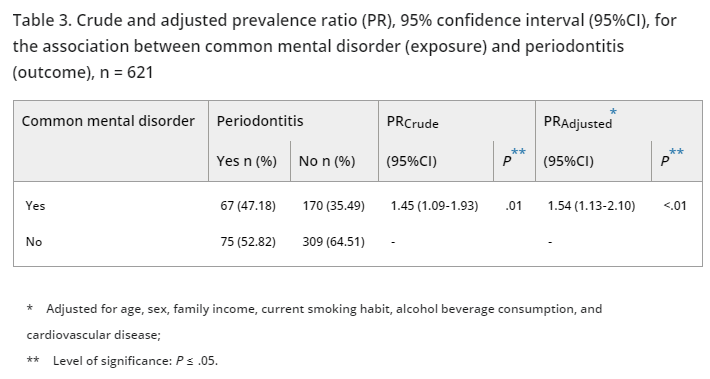
研究纳入了621名参与者,收集一般问卷和诊断CMD的自我报告问卷数据。根据全口牙周检查,包括临床附着水平、探诊深度和探诊出血,诊断牙周炎。获得CMD(暴露)和牙周炎(结果)之间的患病率比和95%置信区间。
结果,在最终样本中,38.16%(237名参与者)的参与者诊断为CMD。其中,28.27%(67名参与者)名参与者患有牙周炎。关联测量结果显示,校正年龄、性别、家庭收入、目前的吸烟习惯、酒精饮料消费和心血管疾病后,暴露于CMD的人群中牙周炎的发生率比没有这种精神状况的人群高出约50%,差异具有统计学意义(校正PR=1.54,95%CI:[1.13~2.10])。
综上所述,该研究结果显示,CMD和牙周炎之间存在正相关关系,提示扩大针对心理健康公共行动的重要性,而结果可能是由于研究样本中心理疾病的高患病率。
原始出处:
Julita Maria F Coelho, Samilly S Miranda, et al., Common mental disorder is associated with periodontitis. J Periodontal Res. 2020 Apr;55(2):221-228. doi: 10.1111/jre.12705. Epub 2019 Oct 28.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#发病率#
67
#精神障碍患者#
66
#PE#
56
学习学习
116
#牙周#
93