容易漏诊、误诊的主动脉夹层
2016-07-24 赵永祯 首都医科大学附属北京朝阳医院 急诊科 医学界急诊与重症频道
1 . 病例资料患者,男性,62 岁,因“腹痛、腹泻1天,左下肢无力3小时”于急诊就诊。患者近1天无明显诱因出现上腹部钝痛伴呕吐2次胃内容物,并有腹泻3次,为黄稀便。3 小时前出现左下肢无力、感觉麻木,无腿痛,无头痛、无胸背痛。既往有冠心病、心梗,及胰腺炎病史,否认有高血压、糖尿病及手术外伤史。查体:体温 36℃,心率 79 次/分,呼吸 18 次/分,右上肢血压 148/84 mmHg,左上
1 . 病例资料
患者,男性,62 岁,因“腹痛、腹泻1天,左下肢无力3小时”于急诊就诊。患者近1天无明显诱因出现上腹部钝痛伴呕吐2次胃内容物,并有腹泻3次,为黄稀便。3 小时前出现左下肢无力、感觉麻木,无腿痛,无头痛、无胸背痛。既往有冠心病、心梗,及胰腺炎病史,否认有高血压、糖尿病及手术外伤史。
查体:体温 36℃,心率 79 次/分,呼吸 18 次/分,右上肢血压 148/84 mmHg,左上肢血压 145/80 mmHg;神志清楚,言语流利;双肺呼吸音粗,未闻罗音;心律齐,心音低,各瓣膜听诊区未闻及明显杂音;腹平软,左上腹压痛(+),无反跳痛、肌紧张,肝脾未及;左下肢肌力 Ⅲ级,余肢体肌力 V级,双巴氏征(-),双足皮温正常,可触及足背动脉搏动。
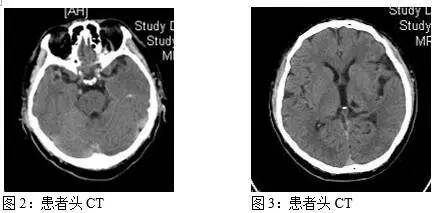
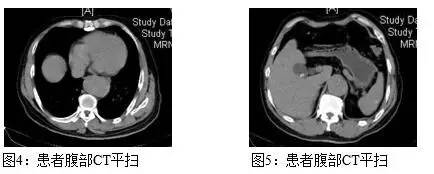
来院后半小时内检查结果显示,血常规:WBC 20.86*109/L、N 92.1%、HGB 168 g/L、HCT 47.3%、PLT 137*109/L;尿常规:红细胞(++++)、白细胞(+)、酮体(+)、尿蛋白150 mg/L(+++)、葡萄糖 100 mg/dl(++);尿胰蛋白酶原II阳性;心电图见图1;头颅CT平扫:桥脑、左侧基底节、左侧丘脑腔隙性脑梗塞;轻度老年性脑改变。脑动脉硬化(图2、3)。暂先予抗炎补液治疗,并同时行全腹 CT 平扫检查。全腹CT提示:胆囊阳性结石,胆囊炎;胸段降主动脉增粗,腹主动脉及其分支多发钙化斑(图4-7)。
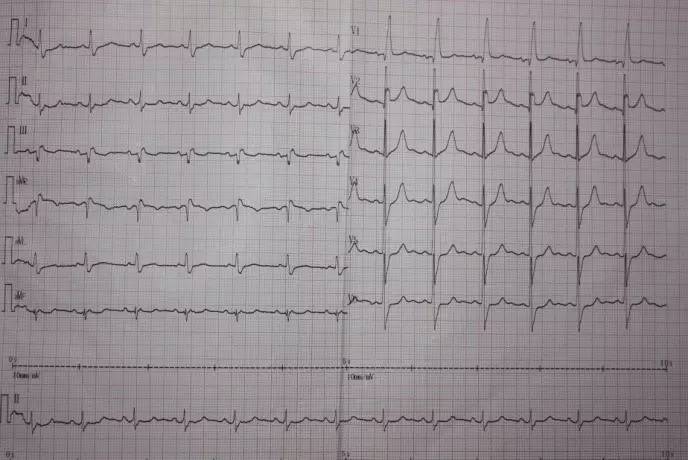
图1:患者心电图

患者来院后两小时,自诉腹痛有减轻,左下肢肌力有好转,查体左下肢肌力为V-级。此时化验结果显示:肌酸激酶1267 U/L、肌酸激酶同工酶 31.1 ng/ml、心肌钙蛋白 10.17 ng/ml,血淀粉酶 513 U/L,D-二聚体 35.20mg/L。
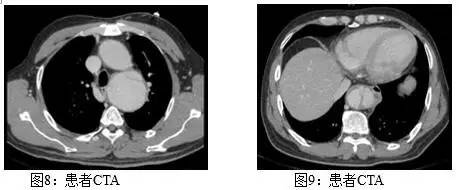
行腹部血管超声可见:腹主动脉内可见条带状高回声分成双腔;提示:腹主动脉夹层可能。患者心电监护显示心率 81 次/分,呼吸 18 次/分,右上肢血压 151/89 mmHg,左上肢血压 148/86 mmHg,予降压药物静点治疗。急行全主动脉增强CT(CTA)检查,CTA诊断:主动脉夹层,累及降主动脉弓、胸主动脉、腹主动脉、双侧髂总动脉(图8-10)。

患者来院后四小时,突然意识不清,血压测不出。再行床旁B超检查提示左侧胸腔大量积液。经抢救无效,患者死亡。
2. 诊断思路
患者腹痛、腹泻后出现单侧下肢无力,如果简单的以胃肠炎、胆囊炎或胰腺炎合并脑血管病来诊断就会造成误诊。而患者的血压和疼痛的表现不典型均给早期诊断主动脉夹层造成困难。患者 D-二聚体的升高和 CT 影像学上的血管改变是早期诊断主动脉夹层的重要依据。
3. 讨论
主动脉夹层临床表现多种多样,疼痛是最常见的症状, 突发严重的胸或及背痛是急性主动脉夹层的特征性表现, 将近90%的急性主动脉夹层患者在急诊就诊时主诉剧烈疼痛, 但也有一小部分患者有轻微疼痛甚至根本无疼痛[1]。据报道有5%一15%的主动脉夹层患者并没有疼痛表现,而以神经系统症状为主要临床表现[2,3]。
根据目前文献的报道,主动脉夹层所引起的神经系统症状的主要发病机制及表现可以分为 3 类[4]:
(1) 主动脉弓分支血管夹层的进展,血压过低导致的脑灌注减少或夹层假腔压迫神经,表现为短暂性脑缺血发作、脑卒中、短暂性全面遗忘样综合征、缺氧性脑病,癫痫发作、意识障碍、Horner综合征、心因性声带麻痹综合征。
(2) 夹层累及供应脊髓动脉导致脊髓缺血,症状主要为各种脊髓损伤综合征,包括横断性脊髓炎, 进展性脊髓病变,脊髓梗死,脊髓前动脉综合征,截瘫,四肢瘫等。
(3) 神经滋养血管闭塞、夹层假腔压迫神经,出现缺血性神经病(下肢轻瘫、多神经病、单神经病)、缺血性神经丛病、神经压迫综合征。这些症状通常在夹层发病时即出现或者不久就出现。首发症状大多数为神经支配区域的严重疼痛,其次为感觉异常如麻木、发冷,甚至运动障碍。部分病例可仅表现为一过性神经系统症状,可能与夹层进展过程中短暂的动脉闭塞有关。本例患者在治疗两小时后下肢肌力恢复就可能与这一原因有关。
有研究表明,D-二聚体对早期诊断主动脉夹层的敏感性为94%,特异性为40%~100%[5]。急性胸痛患者并伴有D-二聚体升高,应怀疑主动脉夹层可能[6]。本例患者D-二聚体明显升高为我们做进一步检查以确断主动脉夹层提供了依据。
本例患者虽经及时明确诊断,但未来得及进一步治疗便突发夹层破裂出血后死亡,由此可见主动脉夹层病情凶险,变化迅速,及时诊断尤为重要。此外,由于主动脉夹层的临床表现多样,临床医师更应提高警惕,加深对这一疾病的认识,尽量减少误诊的发生。
参考文献
[1]沈洪,姚晨玲,陶振钢,等.361例主动脉夹层的临床分析.中国急救医学,2009,29: 499-502.
[2] Stanley I,Sharma VK,Tsivgoulis G,et a1.Painless aortic dissection with unusual extension into intracranial internal carotid arteries.Cerebrovasc Dis,2007,24:314-315.
[3] Demiryoguran NS,Karcioglu O,Topaooglu H,et a1.Pain1ess aortic dissection with bilateral carotid involvement presenting with vertigo as the chief complaint.Emerg Med J.2006,23:15-18.
[4] Gaul C,Dietrich W,Erbguth FJ.Neurological symptoms in aortic:dissection:a challenge for neurologists.Cerebrovasc Dis,2008,26:1-8.
[5] Marill KA. Serum D-dimer is a sensitive test for the detection of acute aortic dissection: a pooled meta-analysis. J Emerg Med,2008,34:367-376.
[6] Ohlmann P, Faure A, Morel O, et al. Diagnostic and prognostic value of circulating D-Dimers in patients with acute aortic dissection. Crit Care Med,2006,34:1358-1364.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













看的我一脸懵逼
105
文章很好值得关注
107
病历很好,值得学习
138
#漏诊#
76
#主动脉#
85
#动脉夹层#
74
好病例,很有帮助
93