Nat Commun:铁蛋白和老年痴呆有关系?!
2015-05-22 佚名 生物谷
近日,一篇发表于国际杂志Nature Communications上的研究论文中,来自墨尔本大学的一项研究表明,高水平的铁蛋白或许和个体轻度认知损伤向阿尔兹海默氏症过渡直接相关。文章中研究人员对91名认知正常的个体、144有轻度认知损伤的个体及67名阿尔兹海默氏症个体进行了长达7年的研究,研究结果显示,在那些轻度认知损伤个体的脑脊髓液中较高水平的铁蛋白或许和其向阿尔兹海默氏症转换直接相关,而铁蛋白
近日,一篇发表于国际杂志Nature Communications上的研究论文中,来自墨尔本大学的一项研究表明,高水平的铁蛋白或许和个体轻度认知损伤向阿尔兹海默氏症过渡直接相关。
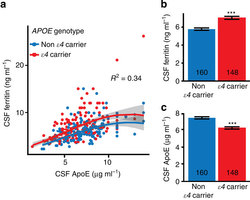
文章中研究人员对91名认知正常的个体、144有轻度认知损伤的个体及67名阿尔兹海默氏症个体进行了长达7年的研究,研究结果显示,在那些轻度认知损伤个体的脑脊髓液中较高水平的铁蛋白或许和其向阿尔兹海默氏症转换直接相关,而铁蛋白和ApoE4基因的存在存在强相关性,ApoE4基因是熟知的阿尔兹海默氏症风险基因。
James Pickett博士表示,此前有研究表明大脑中铁离子的不平衡或许和阿尔兹海默氏症发病相关,而本文研究更增加了此前研究所得的结果;本文研究我们对7年的研究数据进行了分析,结果发现高水平的铁储藏蛋白铁蛋白和个体从轻度认知损伤向阿尔兹海默氏症发病直接相关。
目前研究者并不清楚是否铁离子水平可以被足够准确地用来预测轻度认知损伤向阿尔兹海默氏症的转化,而研究者也不能得出任何结论,即是否我们可以利用铁蛋白来作为未来抑制这种转化的新型靶向疗法;后期研究人员还需要进行更为深入的研究来得到更多的研究结果,从而为开发早期阿尔兹海默氏症发生的新型疗法提供思路。
原始出处:
Scott Ayton,Noel G. Faux,Ashley I. Bush & Alzheimer's Disease Neuroimaging Initiative.Ferritin levels in the cerebrospinal fluid predict Alzheimer’s disease outcomes and are regulated by APOE.Nature Communications, May 19, 2015.doi:10.1038/ncomms7760
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#COMMUN#
76
#Nat#
76
值得期待
128
有意思
141