Diabetes:北京大学杨吉春教授团队发表糖尿病发病机制研究成果
2017-04-20 佚名 生物帮
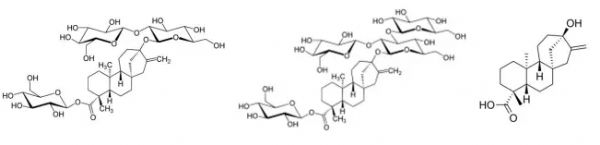
日前,国际内分泌-糖尿病领域的权威期刊《Diabetes》杂志上在线发表了北京大学基础医学院杨吉春教授团队题为“NFE2 Induces miR-423-5p to Promote Gluconeogenesis and Hyperglycemia by Repressing Hepatic FAM3A-ATP-Akt Pathway”和“Hepatic Activation of the FAM
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Diabetes#
68
#机制研究#
90
#北京大学#
79
#DIA#
60
#研究成果#
61
#BET#
53
学习一下谢谢分享
116
拜读了,多谢分享
0