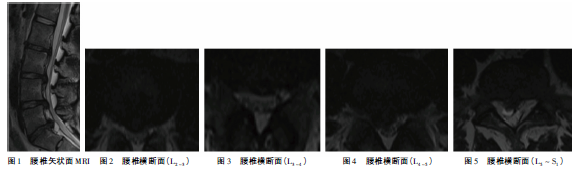
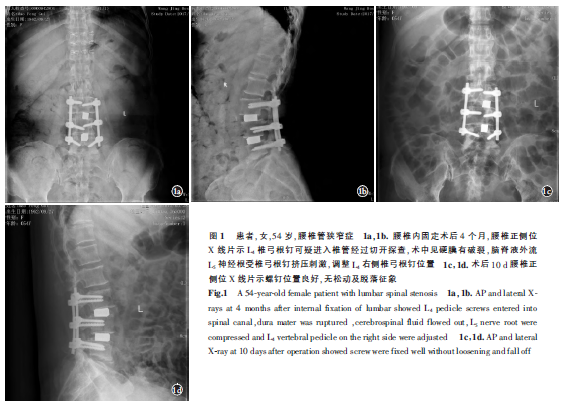
脊柱定点旋转复位法治疗青少年多节段、巨大脱出型腰椎间盘突出症1例
2018-11-26 穆乃旗 郭伟 广西医学
腰椎间盘突出症是现代人群腰腿痛的常见病因,长期劳作、久坐、弯腰负重、外伤等均能导致椎间盘突出,进而压迫神经根,引起一系列神经根受压后引起的临床症状。随着现代生活节奏的加快,腰椎间盘突出症的发病逐渐呈年轻化,而年轻患者在治疗上必然存在一些特殊性,即使椎间盘突出较大,也多采取保守治疗,如针灸、理疗、牵引、药物等,不宜早期手术治疗。本文报告了脊柱定点旋转复位法治疗青少年多节段、巨大脱出型腰椎间盘突出症1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#椎间盘突出#
74
很好的学习机会
102
#腰椎#
53
#腰椎间盘#
57
学习
111
了解一下,谢谢分享!
104