JAMA Oncol :“最毒”乳腺癌生存率提高!精准辅助治疗“复旦方案”登上《美国医学会杂志-肿瘤学》
2020-08-15 药明康德内容团队 医学新视点
乳腺癌中大约15%-20%为三阴性乳腺癌,向来被认为是乳腺癌中最难治、最“毒”的一类。与其他乳腺癌亚型相比,TNBC侵袭性更强,激素或靶向药物都对其效果不佳,全身治疗仍以化疗为主,容易复发转移。
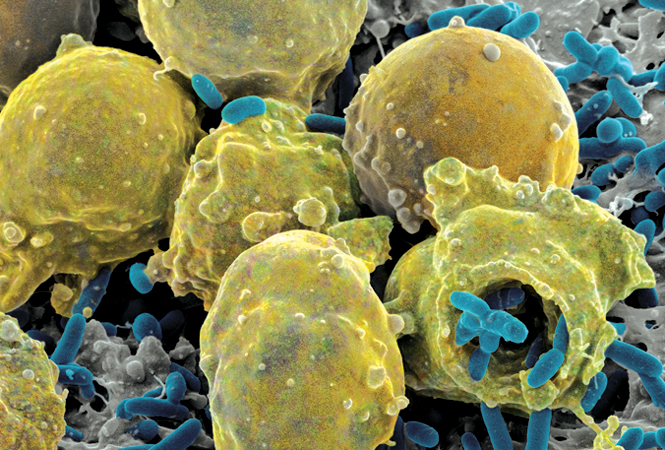
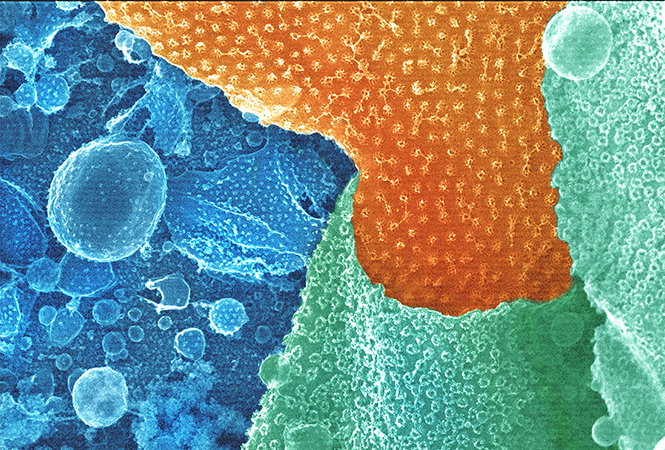
乳腺癌中大约15%-20%为三阴性乳腺癌(TNBC),向来被认为是乳腺癌中最难治、最“毒”的一类。与其他乳腺癌亚型相比,TNBC侵袭性更强,而且由于雌激素、孕激素、HER2三大受体均为阴性,激素或靶向药物都对其效果不佳,全身治疗仍以化疗为主,容易复发、转移。
目前,对于早期TNBC患者,术后辅助治疗的标准方案为蒽环类+紫杉类。然而,标准方案的5年生存率徘徊在80%左右,蒽环类药物还有心脏毒性。如何突破这一瓶颈,基于分子分型来提高TNBC的疗效,是复旦大学附属肿瘤医院团队多年来在牵头攻克的难点。
十年磨一剑,当地时间8月13日,中国研究者发起的PATTERN试验3期结果正式在《美国医学会杂志-肿瘤学》(JAMA Oncology)发表,证明了紫杉醇+卡铂方案在多项生存指标上比标准方案更具优势。论文通讯作者为复旦大学附属肿瘤医院邵志敏教授与余科达教授。研究团队在论文中表示,“这是首次证明,对于早期TNBC患者,含卡铂方案优于蒽环类/紫杉烷方案。”
提出卡铂方案,是因为TNBC通常具有同源重组修复缺陷、基因组不稳定的特点,部分患者出现BRCA通路异常,而铂类药物可能会有效作用于这些机制。已有研究证明含铂方案在TNBC的新辅助治疗或晚期治疗中有效,但在辅助治疗中的价值仍然未得到证明。
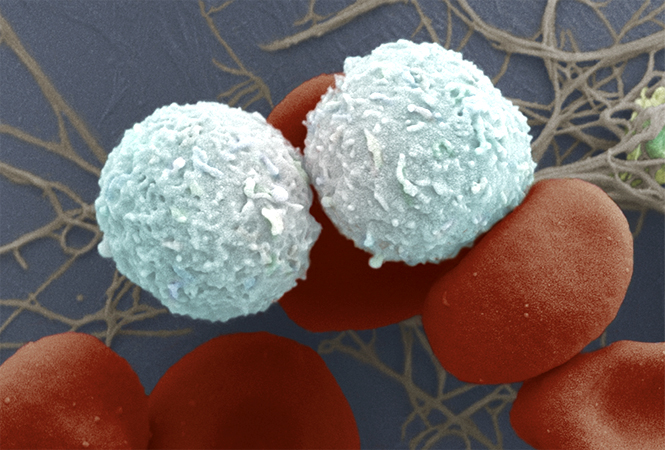
十年前,研究团队提出创新治疗策略后,试验在中国9个临床中心开展,2001年7月-2016年4月期间共纳入了647位可手术的TNBC患者,患者随机分组接受传统标准化疗CEF-T方案(环磷酰胺+表柔比星+氟尿嘧啶+多西他赛,322人)或PCb方案(紫杉醇+卡铂,325人)。
中位随访期为62个月。结果显示:与CEF-T方案相比,接受PCb方案的患者5年无病生存率更高(86.5%vs 80.3%),病变或死亡风险显着降低35%。PCb组患者5年远处无病生存率更高(92.6% vs 87.9%),远处病变或导致死亡风险显着降低41%。PCb组患者5年无复发生存率更高(91.2% vs 84.4%),复发风险显着降低46%。PCb组患者5年总生存比例更高(93.4% vs 89.8%),5年内死亡风险低29%。尽管目前差异不够显着,但论文中指出对总生存期进行更充分的疗效评估将需要更长期的随访。
在亚组分析中,一些特定特征的患者对PCb方案更敏感、生存获益更大:更年轻(<50岁)和肿瘤侵袭性更高的患者。BRCA1/2突变患者,病变或死亡风险降低56%;统计学差异不显着,研究者指出了两点潜在原因:(1)可能是BRCA1/2突变患者样本量较小不足以产生统计效力,(2)即使在BRCA1/2阴性患者中,如果携带同源重组修复相关基因变异也对卡铂敏感。进一步分析也确实表明,同源重组修复相关基因突变患者,病变或死亡风险降低61%。在安全性方面,与相关药物的已知安全性一致。
研究团队在论文最后指出,这些发现表明,紫杉醇+卡铂方案是可手术TNBC患者有效的辅助化疗选择之一;同时,在分子分型时代,值得进一步探索对该方案敏感的TNBC亚组患者,对生物标志物的检测对于选择适合该方案的患者非常重要。
这是复旦大学附属肿瘤医院团队牵头“三阴性乳腺癌精准治疗策略”下的又一重要积极成果,期待对该方案的进一步验证能为患者带来更好、更合适的治疗选择。
原始出处:
Ke-Da Yu, Fu-Gui Ye, Min He, et al.Effect of Adjuvant Paclitaxel and Carboplatin on Survival in Women With Triple-Negative Breast Cancer: A Phase 3 Randomized Clinical Trial.JAMA Oncol. 2020 Aug 13. doi: 10.1001/jamaoncol.2020.2965.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Oncol#
116
#美国医学会杂志#
106
#生存率#
77
#肿瘤学#
122
#精准#
119
#复旦#
84
#三阴性乳腺癌#,紫杉醇+卡铂方案比此前蒽环类/紫杉*方案略有进步,将来可以探索PD-L1+白蛋白紫杉+铂类方案,也许会有一定的突破
237
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
84
谢谢梅斯分享这么多精彩信息
87
哈
143