Lancet neurol:淀粉样脑血管病患者的皮质萎缩:病例对照研究
2016-05-15 MedSci MedSci原创
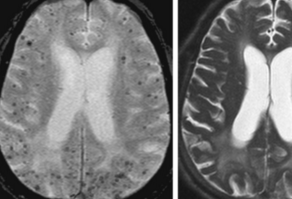
大脑皮层灰质缺失是很多神经退行性疾病的诊断标志,是认知功能障碍的重要介质。我们假定以皮质血管淀粉样蛋白沉积为特征的淀粉样脑血管病(CAA)与阿兹海默病的脑实质病变的病理不同,是皮质组织的缺失。我们在淀粉样变——荷兰型(HCHWA-D)遗传性脑出血患者中(一种单基因疾病伴随最小的或无阿兹海默病病理)、散发CAA患者中验证假说,以健康人群和阿兹海默病患者作为对照。
大脑皮层灰质缺失是很多神经退行性疾病的诊断标志,是认知功能障碍的重要介质。我们假定以皮质血管淀粉样蛋白沉积为特征的淀粉样脑血管病(CAA)与阿兹海默病的脑实质病变的病理不同,是皮质组织的缺失。我们在淀粉样变——荷兰型(HCHWA-D)遗传性脑出血患者中(一种单基因疾病伴随最小的或无阿兹海默病病理)、散发CAA患者中验证假说,以健康人群和阿兹海默病患者作为对照。
这个病例对照研究将受试者分为6组:经基因检测诊断为HCHWA-D的患者组;健康对照组,年龄与HCHWA-D组相匹配;可能患有散发的CAA而无痴呆;健康对照组两个独立的队列,年龄与CAA组相匹配;阿兹海默病患者组,年龄与CAA组匹配。队人口、临床、放射学和遗传数据进行去识别化,数据来源麻省总医院(美国波士顿),莱顿大学(荷兰莱顿)以及阿尔茨海默病的神经影像学(ADNI)网站。主要终点是测量皮层厚度。对皮层厚度和结构病变的相互关系,血氧水平依赖时间峰值 (BOLD-TTP;生理学上用于测量血管功能)进行分析,以此了解血管淀粉样变和皮层厚度的潜在联系的机理。
使用之前验证的计算机辅助工具来量化影像学变化的益处,对所有的结果进行直接观察确保准确性。
在2006年5月15日到2014年12月1日,招募了369位受试者(有26例HCHWA-D患者,与年龄相匹配的健康对照组28人;63例患有散发CAA无痴呆患者;两个健康对照队列分别有63和126人;阿兹海默病患者63例)。
26例 HCHWA-D的患者与28例健康对照组 人群(平均差异−0·112 mm, 95% CI −0·190 to −0·034, p=0·006)相比有更薄的皮层厚度 (2·31 mm [SD 0·18])。63例有散发CAA无痴呆的患者与两个健康对照组(n=63, 平均差异 −0·14 mm, 95% CI −0·17 to −0·10, p<0·0001; n=126, −0·10, −0·13 to −0·06, p<0·0001)相比,有更薄的皮层厚度 (2·17 mm [SD 0·11]) 。
多变量分析后所有的差异仍然独立存在。63例阿兹海默病患者与散发CAA患者 (2·1 mm [SD 0·14], 差异0·07 mm, 95% CI 0·11 to 0·02, p=0·005)相比表现出更加严重的皮质萎缩。我们发现在HCHWA-D患者(ρ=–0·58, p=0·003) 及散发CAA患者(r=–0·4, p=0·015)中,皮质厚度与血管功能障碍有显著的关系,但是在对照组中无关。血管功能障碍是遗传性CAA患者皮质萎缩的重要介导,占总体影响的63%。
结论: HCHWA-D患者皮质变薄表明了血管淀粉样变是皮质萎缩的独立危险因素。这些结果在散发CAA患者中更加常见。我们的研究显示CAA相关皮质萎缩至少有部分原因是由于血管功能障碍介导的。同时支持了小血管疾病即使不合并阿兹海默病,如CAA可以导致皮质萎缩。这些结论可以帮助放射科医生、神经科医生及其他临床医生对老年患者的诊断。
原始出处:
Panagiotis Fotiadis, BS†, Sanneke van Rooden, PhD†,et al, Jeroen van der Grond, Cortical atrophy in patients with cerebral amyloid angiopathy: a case-control study,The Lancet Neurology,Published Online: 11 May 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Lancet#
93
#病例对照#
126
#血管病#
102
#对照#
97
#病例对照研究#
116
#萎缩#
102
#Neurol#
97
这个研究可以学习
208