牛津大学科学家Cell子刊发表两项卵巢癌研究进展
2016-08-02 佚名 生物谷
最近来自英国牛津大学的一支研究团队在EBioMedicine和Cancer Cell两个国际学术期刊上发表了两项卵巢癌研究进展,他们在第一项研究中发现了一个帮助早期检测卵巢癌的标志物分子,并在第二项研究中发现一种使卵巢癌变得更加致命的关键酶,他们的研究为更多科学家检测并击败这种疾病提供了新的研究思路。 在第一项研究中研究人员发现SOX2的蛋白表达水平在卵巢癌患者输卵管中的水平更高,并且在一些卵巢
最近来自英国牛津大学的一支研究团队在EBioMedicine和Cancer Cell两个国际学术期刊上发表了两项卵巢癌研究进展,他们在第一项研究中发现了一个帮助早期检测卵巢癌的标志物分子,并在第二项研究中发现一种使卵巢癌变得更加致命的关键酶,他们的研究为更多科学家检测并击败这种疾病提供了新的研究思路。
在第一项研究中研究人员发现SOX2的蛋白表达水平在卵巢癌患者输卵管中的水平更高,并且在一些卵巢癌高危人群(如BRCA1和BRCA2基因突变携带者)中SOX2的表达水平也会更高。
牛津大学的Ahmed Ashour Ahmed教授表示:“卵巢癌的早期诊断非常困难,有的患者甚至在患病4年后才发现癌症的存在,目前只有三分之一的癌症患者能够得到早期诊断。检测SOX2表达不仅可以帮助更早地发现癌症,而且在一些病例中还可以在肿瘤癌变之前发现肿瘤。早治疗能够大大提高病人的生存几率,因此早发现是非常重要的。但是由于检测输卵管的SOX2表达并不是一件容易的事情,因此我们仍然还有很多工作要做。”
在第二项研究中,该研究团队发现了一种促进卵巢癌细胞扩散的关键酶。当卵巢癌发生扩散,通常会扩散到网膜——覆盖小肠的脂肪组织。卵巢癌患者最常见的死因就是肿瘤生长阻塞肠道导致的营养不良。
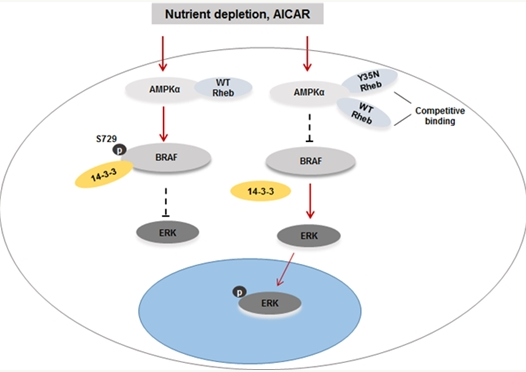
Ahmed教授解释道:“之前研究发现网膜部位的脂肪细胞会产生游离脂肪酸,促进癌症扩散。而我们发现卵巢癌细胞的增殖依赖一种叫做SIK2的关键酶,SIK2对于燃烧脂肪酸产生癌细胞生长所需的能量具有非常重要的作用。我们发现SIK2的表达水平在网膜部位的继发性肿瘤中比卵巢部位的原位肿瘤更高。”
研究表明SIK2不仅在卵巢肿瘤的生长过程中发挥关键作用,还在卵巢肿瘤向网膜的扩散过程中发挥重要作用,这会使卵巢癌变得更加致命。
研究人员表示,SIK2不仅能够为癌细胞提供能量,还会进一步增加癌细胞的数目,因此是未来卵巢癌治疗的一个重要靶点,破坏这种关键酶能够降低癌细胞扩散和癌症复发的可能。
原始出处:
Discoveries offer hope for managing ovarian cancer
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
42
#CEL#
52
#研究进展#
47
#牛津大学#
65
好好学习
93