Ann Intern Med:乳腺密度的评估与其放射科医生有很大关系
2016-07-26 MedSci MedSci原创
目前,美国近一半的州颁布立法要求放射设备公布女性乳腺密度的结果,有些人建议对致密乳腺的女性进行是否需要补充检查进行讨论。 为了验证乳腺密度的评估在放射科医生之间的差异,对收集的观察数据进行了一项横断面和纵向的前瞻性研究。在以人群为基础的个性化方案优选筛查联合 (PROSPR) 研究中的3个乳腺癌放射研究中心的30个放射设备中进行。 放射科专家在2011年到2013年至少审查过500个乳
目前,美国近一半的州颁布立法要求放射设备公布女性乳腺密度的结果,有些人建议对致密乳腺的女性进行是否需要补充检查进行讨论。
为了验证乳腺密度的评估在放射科医生之间的差异,对收集的观察数据进行了一项横断面和纵向的前瞻性研究。在以人群为基础的个性化方案优选筛查联合 (PROSPR) 研究中的3个乳腺癌放射研究中心的30个放射设备中进行。
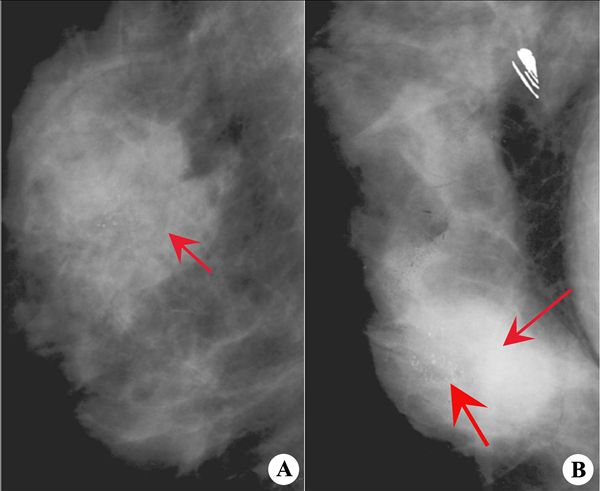
放射科专家在2011年到2013年至少审查过500个乳腺X摄像图片(n = 83)。共包含了145123名年龄40-89岁女性的216 783张乳腺射片。
使用第4版乳腺成像报告和数据系统类别(混合密度和极高密度称为"致密"),同时记录患者年龄,种族,体脂比(BMI)。
结果显示,共有36.9%的乳腺射片被认为是致密乳腺。在不同放射科专家中变化范围是 6.3% 到 84.5%(中位,38.7% [四分位距,28.9%- 50.9%]),对患者特征进行多变量调整后仅有很小的影响(四分位距,29.9% 到50.8%)。患者亚组分析显示放射科专家中对致密乳腺的评估差异普遍存在,主要是和患者的年龄和BMI结合的结果。不同放射科专家进行的连续审片中,17.2% (5909/34 271)对致密有不同的意见vs非致密。
局限性:无法对乳腺射片的密度进行定量测量。
结论:不同放射科专家对乳腺致密性的评估差异较大,决策者和提供者在考虑补充检查策略时应谨慎考虑。女性是否被告知存在致密乳腺与对其审片的放射科医生有很大关系。
原始出处:
Sprague BL, Conant EF, Onega T, Garcia MP, et al,Variation in Mammographic Breast Density Assessments Among Radiologists in Clinical Practice: A Multicenter Observational Study.Ann Intern Med. 2016 Jul 19. doi: 10.7326/M15-2934. [Epub ahead of print]
相关会议推荐
第十二届国际呼吸学会暨ATS联合论坛:http://www.isrd.org/

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#放射科医生#
59
很好,不错,以后会多学习
79
很好,不错,以后会多学习
86
好文章,百姓也能从中学到好多医学知识
107
#放射科#
55
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
102
#乳腺密度#
62
#Med#
50
主观因素多,需要一个标准来操作
84
了解
88