JACC:Ivabradine可有效改善体位性直立性心动过速综合征患者的心率和生活质量
2021-03-02 MedSci原创 MedSci原创
体位性直立性心动过速综合征(POTS)是一种复杂的、多因素疾病,会损害功能状态和生活质量。目前可用的治疗药物有限,Ivabradine是否可有效治疗POTS?
体位性直立性心动过速综合征(POTS)是一种复杂的、多因素疾病,会损害功能状态和生活质量。目前可用的治疗药物有限。
本研究旨在探讨选择性窦房结Ifunny通道阻滞剂伊伐布雷定(ivabradine)对血浆去甲肾上腺素(NE)>600pg/ml和倾斜试验异常的高肾上腺素能POTS患者心率、生活质量(QOL)和血浆NE水平的影响。
这是一项随机、双盲、安慰剂为对照的伊伐布雷定交叉试验,共22例以高肾上腺素能POTS为主要亚型的患者完成了该试验。随机分组后患者接受伊伐布雷定或安慰剂治疗1个月,然后交叉使用另一种治疗1个月。在基线和每个治疗月末测量心率、生活质量和血浆NE水平。
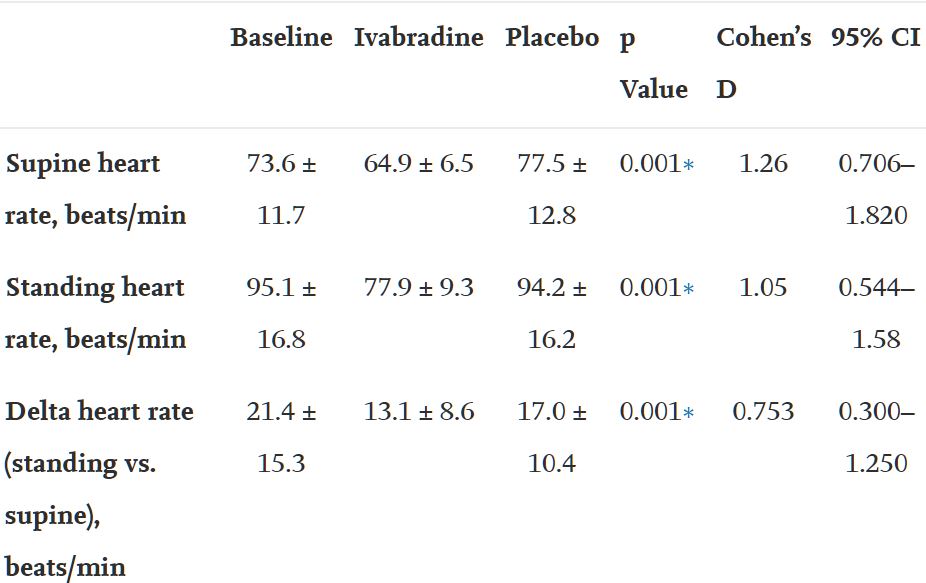
伊伐布雷定对心率的影响
受试患者平均年龄为 33.9±11.7岁,女性占95.5%(n=21),白人占86.4%(n=23)。与安慰剂组相比,伊伐布雷定组患者的心率明显减慢(P<0.001)。
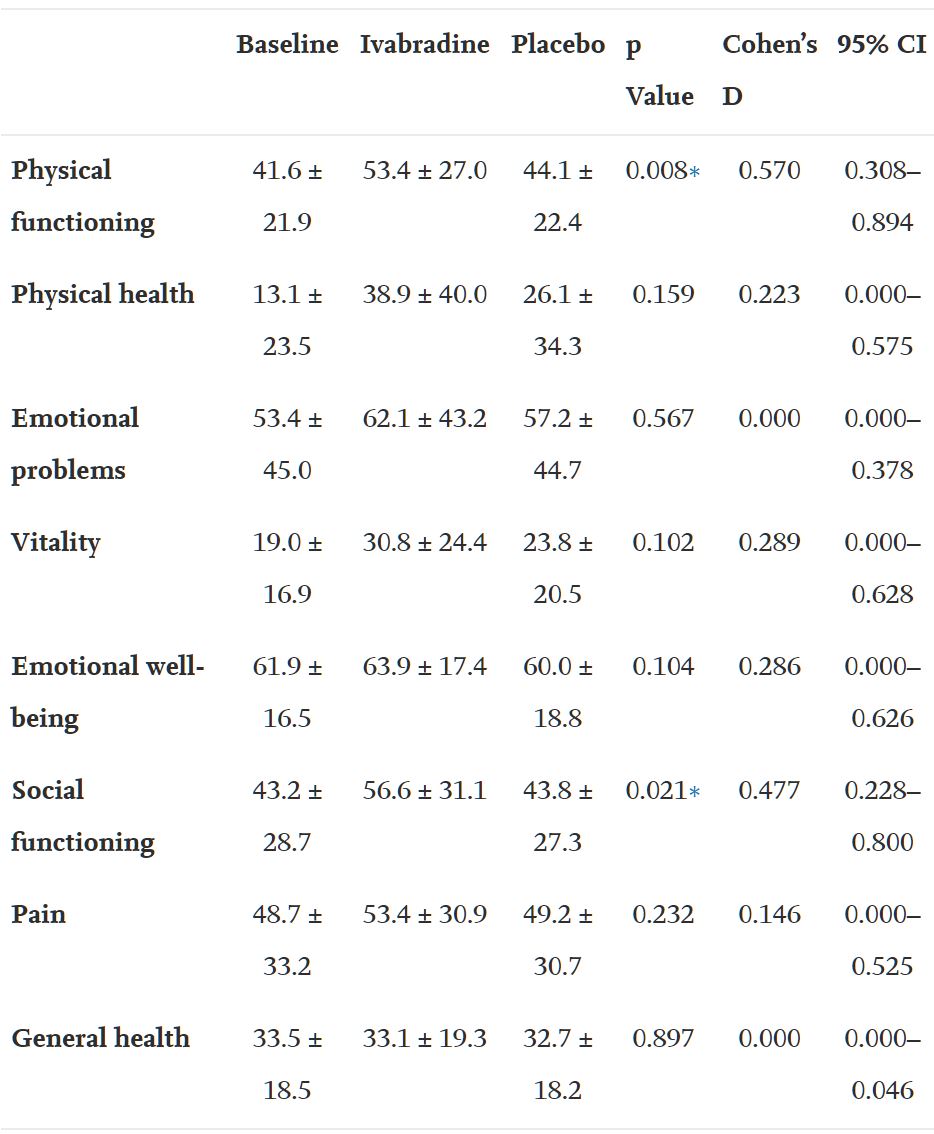
伊伐布雷定对生活质量的影响(SF-36)
通过RAND 36项身体功能和社会功能健康调查1.0,患者报告的的生活质量都有了显著的改善。服用伊伐布雷定后,NE水平有明显下降趋势(p=0.056),且没有出现任何明显的副作用,如心动过缓或低血压。
综上,伊伐布雷定能明显改善以高肾上腺素能POTS为主要亚型的患者的心率和生活质量,是一种安全有效的治疗方法。
原始出处:
Taub Pam R,Zadourian Adena,Lo Hannah C et al. Randomized Trial of Ivabradine in Patients With Hyperadrenergic Postural Orthostatic Tachycardia Syndrome. J Am Coll Cardiol, 2021, 77: 861-871.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JACC#
82
很有用
185
#ACC#
86
#综合征#
0
#心动过速#
73
!
112