Chin Circul J:<6月主动脉缩窄患儿不适于球囊扩张治疗
2017-04-01 朱朱 中国循环杂志
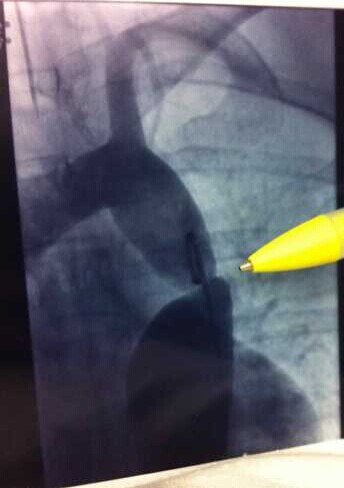
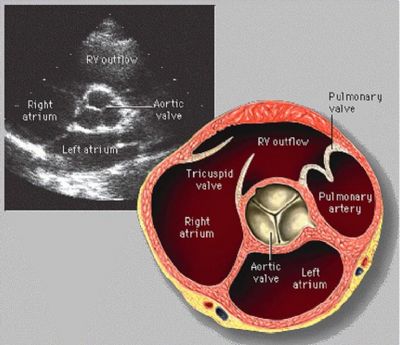
青岛妇女儿童医院邸勇等本刊发文报告,对于6个月以下的主动脉缩窄婴幼儿,球囊扩张治疗效果差,建议用外科手术治疗此类患儿。作者指出,主动脉缩窄球囊扩张对于是否适合婴幼儿治疗仍存在较大争议。目前,很多学者以为对于未曾外科手术治疗的局限性、隔膜型主动脉缩窄患儿球囊扩张效果明显。但作者发现:行球囊扩张后,患儿的主动脉狭窄段直径略有增长,HE 染色示其内层粘膜脱落,但中层平滑肌连续性完整,说明单纯球囊扩张效果
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
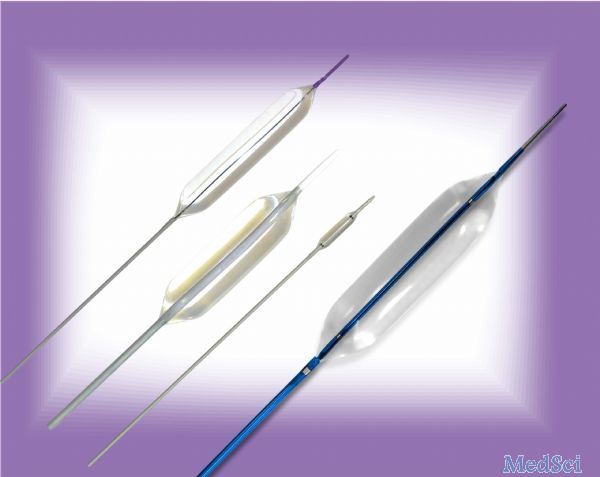









#球囊扩张#
39
#扩张#
43
#主动脉缩窄#
34
#球囊#
36
#主动脉#
38