AHA 2013:小剂量多巴胺或奈西立肽未能改善急性心力衰竭患者肾功能(ROSE AHF研究)
2013-11-20 佚名 丁香园
2013年11月18日,美国心脏协会(AHA)2013科学年会公布的一项急性心衰肾脏最优策略评估(ROSE AHF)研究结果显示,小剂量多巴胺或奈西立肽未能改善急性心衰患者的肾功能。 ROSE AHF研究是一项多中心、双盲、对照、随机临床研究,360例伴肾功能不全的急性心衰(AHF)住院患者随机分为3组,分别给予小剂量多巴胺(2ug/kg/min)、小剂量奈西利肽(0.005ug/kg/mi
2013年11月18日,美国心脏协会(AHA)2013科学年会公布的一项急性心衰肾脏最优策略评估(ROSE AHF)研究结果显示,小剂量多巴胺或奈西立肽未能改善急性心衰患者的肾功能。
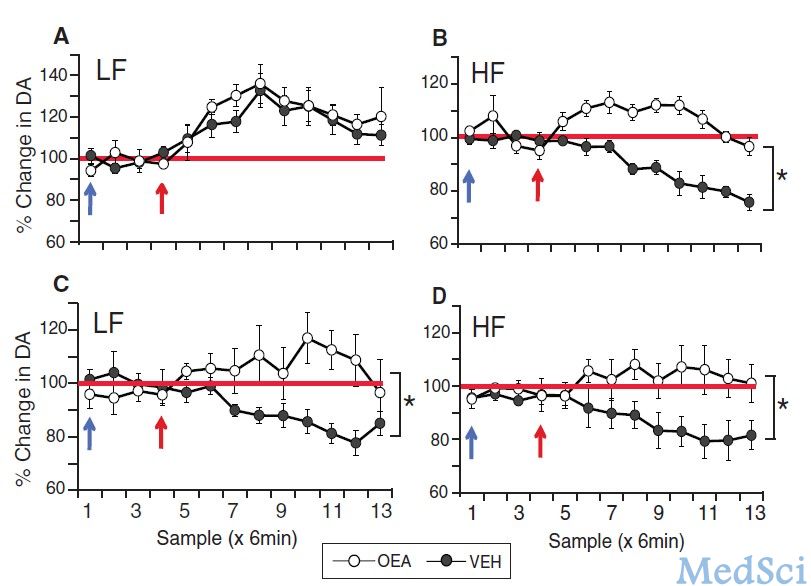
ROSE AHF研究是一项多中心、双盲、对照、随机临床研究,360例伴肾功能不全的急性心衰(AHF)住院患者随机分为3组,分别给予小剂量多巴胺(2ug/kg/min)、小剂量奈西利肽(0.005ug/kg/min)和安慰剂。
研究人员收集患者在基线、24小时、48小时、72小时、7天或出院、60天和6个月的检测数据,发现在标准治疗基础上,加用两种药物在增加尿量或改善血清胱抑素C(肾功能标志物)方面均不优于安慰剂。
“既往有小规模临床研究表明小剂量多巴胺或小剂量奈西利肽能够改善AHF患者的肾功能,减轻心脏充血。但目前FDA尚未批准这两种药物用于改善AHF患者的肾功能。我们的研究结果并未证明这一结论”,Mayo 诊所的Horng Chen博士介绍说,“在一些患者亚组中,这两种药物的反应有所不同”,然而总体效果和安慰剂无显著差异。急性心衰患者的血压和心功能差异很大,关于急性心衰的进一步研究应当评估不同患者亚组的治疗”。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









很不错的文章
122
这两种药物的反应有所不同
199
#肾功能#
73
#AHF研究#
68
#AHF#
87
#小剂量#
64
#AHA#
56
#急性心力衰竭#
82
#ROS#
56