Angew Chem & J Biophotonics:开发出新型血液阿尔茨海默病诊断方法
2016-03-17 佚名 生物谷
目前,阿尔茨海默病(AD)诊断太晚了。在一项新的研究中,来自德国神经退行性疾病中心(DZNE)和波鸿大学(RUB)等机构的研究人员开发出一种血液测试,可能加快在早期阶段检测阿尔茨海默病。它利用红外传感器进行免疫化学分析。这种传感器的表面包被高度特异性的抗体,从而能够捕获来自血液或脑脊髓液中的阿尔茨海默病生物标志物。这种传感器分析这些生物标志物是否已反映了病理变化,其中这些病理变化能够在任何
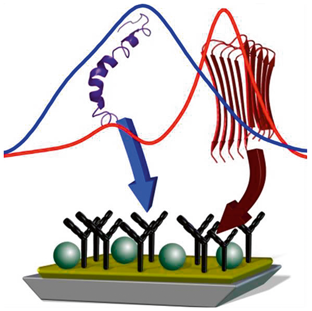
目前,阿尔茨海默病(AD)诊断太晚了。在一项新的研究中,来自德国神经退行性疾病中心(DZNE)和波鸿大学(RUB)等机构的研究人员开发出一种血液测试,可能加快在早期阶段检测阿尔茨海默病。它利用红外传感器进行免疫化学分析。这种传感器的表面包被高度特异性的抗体,从而能够捕获来自血液或脑脊髓液中的阿尔茨海默病生物标志物。这种传感器分析这些生物标志物是否已反映了病理变化,其中这些病理变化能够在任何临床症状出现15多年前发生。这种方法作为2016年3期封面文章发表在国际知名的学术期刊 Journal of Biophotonics上,这项研究的结果也发表在Analytical Chemistry期刊上,论文标题分别为“An infrared sensor analysing label-free the secondary structure of the Abeta peptide in presence of complex fluids”和“Amyloid-β-Secondary Structure Distribution in Cerebrospinal Fluid and Blood Measured by an Immuno- Infrared-Sensor: A Biomarker Candidate for Alzheimer’s Disease”。
在大多数阿尔茨海默病病例中,诊断太晚了
阿尔茨海默病诊断的一个主要问题在于当临床症状首次出现时,大规模不可逆的脑损伤已经发生。在这个时候,对症疗法是唯一的可用选择。波鸿大学生物物理系主任Klaus Gerwert教授说,“如果我们想要一种能够显著地抑制这种疾病发展的药物供我们使用,那么我们需要能够在早期检测阿尔茨海默病的血液测试方法。” 德国哥廷根大学精神病学与心理治疗系主任Jens Wiltfang教授补充道,“通过在早期使用这种药物,我们可能能够阻止痴呆症,或者至少延缓它的发生。”
阿尔茨海默病与β-淀粉样肽错误折叠
对这项新的测试而言,β-淀粉样肽(Amyloid beta peptide)的二级结构充当着生物标志物的作用。在阿尔茨海默病病人体内,这种结构发生变化。在这种错误折叠的病理结构中,越来越多的β-淀粉样肽能够堆积,逐渐在大脑中形成可观察到的斑块沉积,它也是阿尔茨海默病的典型特征。这种变化在临床症状首次出现15多年前就已发生。这种病理性的β-淀粉样肽斑块能够被正电子发射断层成像(PET)暂时地检测到,但是这种检测方法相对而言比较昂贵,而且伴随着放射暴露。
已申请专利的阿尔茨海默病诊断方法
在这项研究中,Klaus Gerwert教授领导的一个研究团队与Jens Wiltfang教授一起开发出一种检测β-淀粉样肽错误折叠的红外传感器。这种传感器捕获来自体液中的β-淀粉样肽。这种方法已被提交专利申请。在起初用于脑脊髓液检测后,研究人员随后利用它的方法进行血液检测。Gerwert说,“我们不只是选择β-淀粉样肽的单个可能的折叠结构;相反,我们检测了所有既有的β-淀粉样肽二级结构在正常折叠时和病理性折叠时是如何分布的。”只有对所有二级结构都进行评估才有可能进行精确诊断。已有利用所谓的酶联免疫吸附测试(ELISA)检测β-淀粉样肽的测试方法。它们能够定量检测体液中β-淀粉样肽总浓度、不同长度的β-淀粉样肽所占百分比以及单个β-淀粉样肽构象的浓度,但是它们不能一次提供β-淀粉样肽二级结构诊断相关性的分布信息。Klaus Gerwert.解释道,“这就是当实际用于血液分析时,ELISA测试已被证实并不是那么有效的原因。”
完成首次临床试验
利用这种新开发出的方法,研究人员分析了141名病人的样品。相比于临床上的金标准方法,这种新方法的血液测试精确度为84%,脑脊髓液精确度为90%。这种测试方法揭示出增加的β-淀粉样肽错误折叠会让β-淀粉样肽谱带移动到阈值以下,因而基于此就可诊断阿尔茨海默病。它的独特之处在于它是唯一稳健的、无标记的且只有单个阈值的测试方法。
潜在用于早期检测的传感器
作为这项研究的一部分,研究人员在小群病人中测试了这种新方法在早期阶段检测阿尔茨海默病的潜力。研究结果提示着即便是在早期阶段(痴呆症状尚未出现),也能够在体液中检测到浓度增加的β-淀粉样肽错误折叠。因此,在未来,在临床前期(即症状尚未出现)诊断阿尔茨海默病是可能的。Jens Wiltfang教授补充道,“更早地检测阿尔茨海默病,治疗机会就更好。”当前,针对800名参与者早期检测的样品分析正在进行中,以便更能体现统计学意义。
原始出处:
Andreas Nabers, Julian Ollesch, Jonas Schartner,et al.Amyloid-β-Secondary Structure Distribution in Cerebrospinal Fluid and Blood Measured by an Immuno-Infrared-Sensor: A Biomarker Candidate for Alzheimer's Disease.Anal Chem, 2016, 88 (5):2755–2762.
Nabers A., Ollesch J., Schartner J, et al.An infrared sensor analysing label-free the secondary structure of the Abeta peptide in presence of complex fluids.Journal of Biophotonics.23 MAR 2015.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#IOP#
63
#诊断方法#
68
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
64
#阿尔茨#
52
#photo#
52
#阿尔茨海#
53
#tonic#
58
#Bio#
73
#Angew#
79
#阿尔茨海默#
49