JCO:拉帕替尼+希罗达VS赫赛汀+希罗达用于Her-2阳性转移性乳腺癌
2015-02-03 MedSci MedSci原创
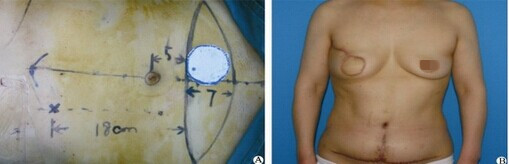
目的:CEREBEL试验对比了Her-2阳性患者在接受“拉帕替尼+希罗达”治疗或接受“赫赛汀+希罗达”治疗后出现疾病复发且以中枢神经系统转移为最先表现的发生率。 材料和方法:无中枢神经系统转移的乳腺癌患者按1:1的比例,随机分为“拉帕替尼+希罗达”组和“赫赛汀+希罗达”组。前者每天服用1250mg拉帕替尼+每21天的1至14天口服希罗达2000mg/m2;后者赫赛汀首次剂量为8mg/kg,之后是
目的:CEREBEL试验对比了Her-2阳性患者在接受“拉帕替尼+希罗达”治疗或接受“赫赛汀+希罗达”治疗后出现疾病复发且以中枢神经系统转移为最先表现的发生率。
材料和方法:无中枢神经系统转移的乳腺癌患者按1:1的比例,随机分为“拉帕替尼+希罗达”组和“赫赛汀+希罗达”组。前者每天服用1250mg拉帕替尼+每21天的1至14天口服希罗达2000mg/m2;后者赫赛汀首次剂量为8mg/kg,之后是每3周输注一次赫赛汀,剂量为6mg/kg。本试验的主要研究终点是以中枢神经系统转移为复发第一站的发生率。次要研究终点是PFS和OS。
结果:本试验总共入组了540名患者,其中271名为“拉帕替尼+希罗达”组,269名为“赫赛汀+希罗达”组。“拉帕替尼+希罗达”组患者发生以中枢神经系统转移为复发第一站的概率为3%,而“赫赛汀+希罗达”组为5%(95%CI,-2% to 5%,P=0.360)。“赫赛汀+希罗达”组相对于“拉帕替尼+希罗达”组患者的OS和PFS较长一些(HR for PFS 1.30 95%CI 1.04 to 1.64;HR for OS 1.34 95%CI 0.95 to 1.64)。严重不良反应的发生率在“拉帕替尼+希罗达”组为13%,在“赫赛汀+希罗达”组为17%。
结论:在本试验中,主要研究终点即以中枢神经系统转移为复发第一站的发生率在“拉帕替尼+希罗达”组和“赫赛汀+希罗达”组之间无显著性差异。“赫赛汀+希罗达”组患者的预后较对照组稍好一些。然而,“拉帕替尼+希罗达”组的疗效可能受到之前因远处转移,患者接受以“赫赛汀”为基础的一线或二线方案的治疗影响。
原始出处
Pivot X1, Manikhas A2, Żurawski B2, Chmielowska E2, Karaszewska B2, Allerton R2, Chan S2, Fabi A2, Bidoli P2, Gori S2, Ciruelos E2, Dank M2, Hornyak L2, Margolin S2, Nusch A2, Parikh R2, Nagi F2, DeSilvio M2, Santillana S2, Swaby RF2, Semiglazov V2.CEREBEL (EGF111438): A Phase III, Randomized, Open-Label Study of Lapatinib Plus Capecitabine Versus Trastuzumab Plus Capecitabine in Patients With Human Epidermal Growth Factor Receptor 2-Positive Metastatic Breast Cancer.J Clin Oncol. 2015 Jan 20.
本文是MedSci原创,欢迎转载,转载请注明出处,非常感谢!

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JCO#
79
#希罗达#
76
#转移性#
53
#赫赛汀#
70
#拉帕替尼#
78
#HER-2#
74
拉帕替尼组患者CNS转移为复发第一站的概率为3%
赫赛汀组患者CNS转移为复发第一站的概率为5%
166
拉帕替尼组口服希罗达2000mg/m²
赫赛汀组口服希罗达2500mg/m²
146
赫赛汀,太厉害!
186
嗯(⊙_⊙)
156