Micell Technologies公布MiStent积极的五年期临床数据
2016-11-01 佚名 Micell Technologies
Micell Technologies在2016TCT年会上公布MiStent积极的五年期临床数据
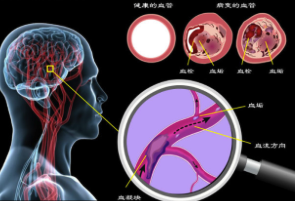
在“Emerging Bioresorbable Polymer-Based Metallic DES”专题会议中,公布了DESSOLVE I和DESSOLVE II临床研究的五年期结果,显示两项研究五年的靶病变血运重建率(TLR)为2.7%。在五年的随访中,两项研究均未出现可能或明确的支架内血栓形成。研究结果由佐治亚州亚特兰大 Piedmont Heart Institute 介入心脏病学研究主任、医学博士David E. Kandzari公布。
Kandzari博士表示:“来自DESSOLVE I和DESSOLVE II的这些结果证明了我们最初的假设,MiStent独特的药动学参数,加上快速吸收的聚合物和更强的结晶型西罗莫司洗脱,可实现快速稳定的血管愈合,带来非常好的长期效果。”
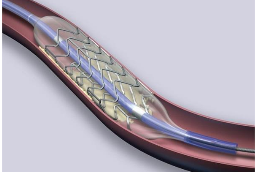
俄亥俄州辛辛那提基督医院心血管中心和Lindner研究中心医务主任、医学博士Dean J. Kereiakes也通过展板报告介绍了五年期结果的相关数据。Kereiakes博士表示:“MiStent采用线性药物释放和超薄钴铬支架设计,这项关于接受MiStent治疗的患者的汇总分析表明,这种新型冠状动脉支架具有极佳的长期安全性和有效性。”
Micell已获专利的超临界流体技术可进行严格控制的药物和聚合物涂层,从而将干粉状、结晶型药物应用于裸金属支架。这不仅保留了其形态,还优化了其药动学(分布和吸收)参数。MiStent还利用了钴铬冠状动脉支架系统的好处,而这款一流的超薄金属支架经证明具有卓越的递送性、顺应性和灵活性。
Micell首席医学顾问、医学博士Dennis Donohoe表示:“MiStent提供长达9个月的持续血管给药,即使是在其生物可吸收聚合物涂层被完全吸收以后,而这需要90天的时间。”Donohoe博士接着说:“迄今为止所进行的MiStent研究已经证明18个月的晚期管腔丢失令人满意,这使得MiStent对于治疗冠状动脉疾病患者而言是一个具有临床意义的改进。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#TEC#
59
#临床数据#
83
#Stent#
67
#CEL#
68
#Cell#
76
好好好赞学习
86