Age aging:运动少、高血压和低学历是我国痴呆三大原因!中国25万人分析
2020-04-26 xujing 中国循环杂志
近期,一项研究提示,运动少、高血压和低学历是我国老年痴呆的三大原因。
中国是世界上痴呆人数最多的国家,痴呆人数从1990年的368万人增加到2010年的919万人。
根据中国疾病负担报告,作为痴呆的最重要分型,阿尔兹海默症死亡增幅62.4%。
近期,一项研究提示,运动少、高血压和低学历是我国老年痴呆的三大原因。
研究还显示,55%的痴呆可归因于中年肥胖、缺乏运动、吸烟、低学历、糖尿病、高血压和抑郁症七个危险因素。
在2010年,这些危险因素导致超过500万人痴呆。
研究发现,痴呆患者中,有82.2%身体活动不足、79.3%学历低,33.8%为高血压。
然而,抑郁致导致痴呆的危险性最高(RR=2.08),其次是高血压(RR=1.84)、糖尿病(RR=1.62)和身体活动不足(RR=1.39)。
研究发现,24.3%的痴呆可归因于身体活动不足,22.1%可归因于高血压,11.9%归因于低学历。
糖尿病(6.3%)、抑郁(4.2%)、吸烟(2.4%)和肥胖(1.1%)也对痴呆有一定影响。
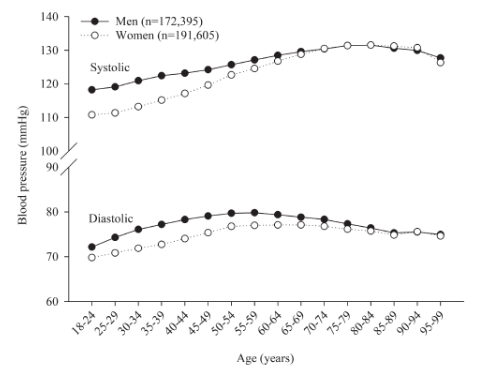
60-69岁老年人群中,48.0%有高血压;61.1%的>70岁老年人有高血压。在这两个年龄段人群,28.7%的痴呆和33.9%的痴呆归因于高血压。
研究者认为,加强体育锻炼,控制高血压,提高全民教育水平,有助于降低我国老年痴呆症的发病率。
这是首次在中国人群中评估痴呆七个危险因素的影响。利用最新的全国调查计算七个风险因素的人口归因分数。
本研究共纳入3项全国性调查,获得7个危险因素的患病率数据:中国慢性病和危险因素监测调查(2013年),覆盖31个省约17万名年龄≥18岁的成年人;(2) 中国慢性肾脏病国家调查(2010年),覆盖13个省约5万名年龄≥18岁的成年人;(3)中国家庭小组研究调查(2012年),覆盖25个省约3万名年龄≥18岁的成年人。
原始出处:Liu Y, Zhang S, Tomata Y, et al. The impact of risk factors for dementia in China. Age Ageing. published online ahead of print, 2020 Apr 21.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











在
134
学习了,非常好!
165
确实如此,可控因素那么多,大有可为
151
学习了,学习了
124
老年人痴呆何药可用??
129