Blood:临终关怀医院,若允许缓解性输血,可很大限度的提高为白血病患者提供的服务质量
2018-06-01 MedSci MedSci原创
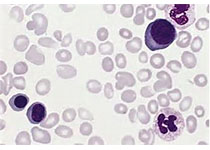
临终医院提供高质量的临终关怀,但白血病患者享受临终服务的频率低于实体肿瘤患者。输血依赖(TD)或许会阻碍或推迟登记,因为临终关怀组织通常不允许输血。Thomas W. LeBlanc等人在享有医疗保险的白血病患者中评估TD和临终结局的关系。研究人员从监察、流行病学和临终医疗数据库中检索死于2001-2011年的医疗受益的急慢性白血病患者。TD定义:死亡或临终关怀登记前30天内输血两次及以上。评估指
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












a:¥CnTwb1llNAq¥
129
#输血#
71
#临终关怀#
101
#临终#
87
一起学习学习
139