Clin Oral Investig:免疫组化分析成釉细胞瘤中的BRAF V600E突变
2018-06-03 lishiting MedSci原创
这篇研究的目的是通过关联个案研究中临床和影像数据,检测下颌骨成釉细胞瘤中BRAF V600E突变的情况。
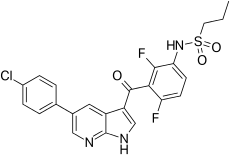
这篇研究的目的是通过关联个案研究中临床和影像数据,检测下颌骨成釉细胞瘤中BRAF V600E突变的情况。研究收集了84例诊断为下颌骨成釉细胞瘤的病例进行分析。样本通过免疫组化检测是否存在BRAF V600E突变的蛋白。同时,收集临床和病理数据:年龄、性别、肿瘤大小、肿瘤在下颌骨的位置、放射线影像结果、组织学类型和亚型以及肿瘤状态。基于BRAF V600E的检测,将临床-病理参数进行分类和分析。结果显示,84名患者中,有78.6% (66例)展现出抗BRAF V600E抗体阳性,有18 (21.4%)例表现出阴性。BRAF的表达和变化之间的联系显示出下颌骨的位置(P=0.0353)和肿瘤大小(P=0.008)与其存在明显关联,而年龄、性别、放射线影像结果、组织模式、组织学亚型以及肿瘤状态没有显著意义。多变量logistic回归分析表明,BRAF阳性在下颌骨靠后的部位(OR=7.23, P=0.0451)以及大小>4 cm (OR=7.29, P=0.0150)的肿瘤存在明显风险。结论:BRAF V600E突变通常发生在下颌骨的成釉细胞瘤中,特别是在肿瘤大于4 cm以及发生在下颌骨靠
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oral#
112
#V600E突变#
76
#成釉细胞#
85
#EST#
69
#BRAF#
106
#免疫组化#
77
#细胞瘤#
71
学习学习谢谢
126
学习
90
学习了.长知识
133