盘点:9月卵巢癌指南共识及重大成果一览
2016-10-03 MedSci MedSci原创
众所周知,卵巢恶性肿瘤是女性生殖器官常见的恶性肿瘤之一,发病率仅次于子宫颈癌和子宫体癌而列居第三位。但卵巢上皮癌死亡率却占各类妇科肿瘤的首位,对妇女生命造成严重威胁。这里小M盘点了9月份与卵巢癌相关的重要研究进展与大家分享。一、重大成果1,Br J Cancer:饮食中的多氯联苯会不会增加乳腺癌、子宫内膜癌和卵巢癌风险?多氯联苯(PCB)暴露对激素相关的癌症风险有什么影响?目前的观察性研究得出
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言





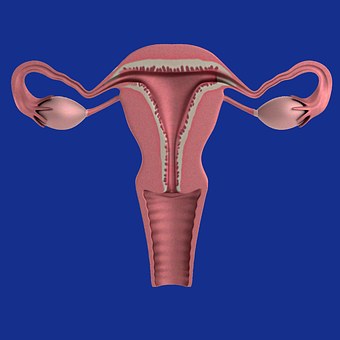








众所周知,卵巢恶性肿瘤是女性生殖器官常见的恶性肿瘤之一,发病率仅次于子宫颈癌和子宫体癌而列居第三位。但卵巢上皮癌死亡率却占各类妇科肿瘤的首位,对妇女生命造成严重威胁。
101
好文章,受益
100
文章很好,继续关注
97
文章很好,继续关注
122
学习了,谢谢分享,继续关注中
98
天天早上
54
认真学习
75
好好看书
61
好好玩
0
很高兴能有梅斯医学
64