Cell Stem Cell:神经再生又添大实锤!科学家在近百岁的AD患者脑中,发现神经再生,且再生水平与认知能力正相关
2019-05-31 奇点糕 奇点网
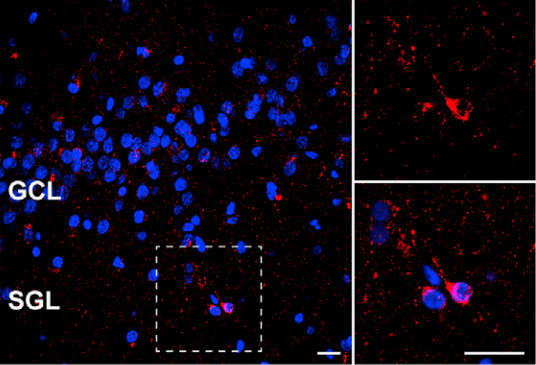
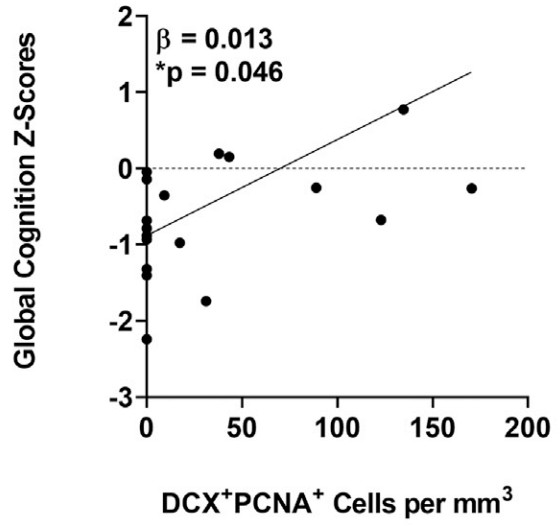
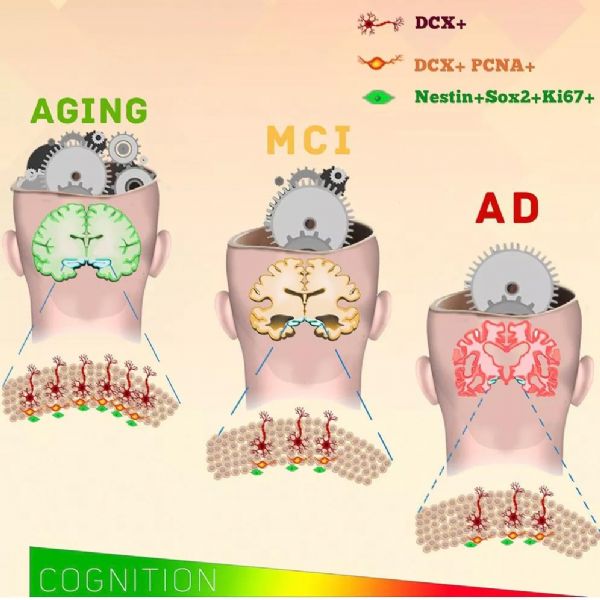
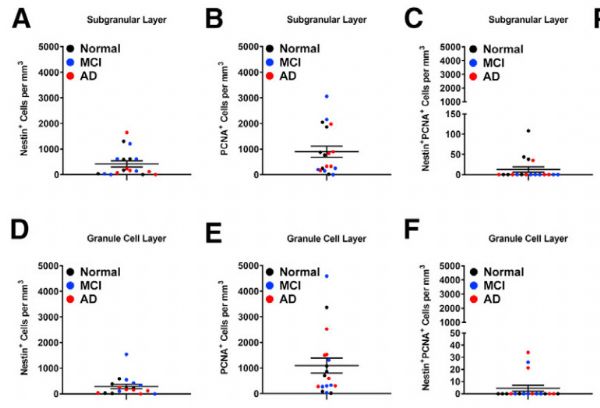
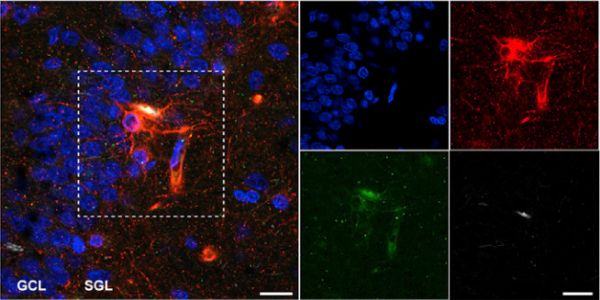
神经细胞,多年以来一直被认为是不可再生的,死一个就少一个。然而在2个月前,马德里自治大学的科学家们在老年人的大脑中发现了新生的神经元,动摇了神经细胞不可再生的理论。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CEL#
97
#stem cell#
50
#Cell#
48
#正相关#
66
#STEM#
99
#神经再生#
93
向科研人员致敬!
100
学习
116