Nat Commun:新进展!抑制TMBIM6基因可抑制原发性肿瘤的生长
2020-08-18 Lauren 转化医学网
导言:肿瘤标志物在1978年就被发现了,它是指在血液、体液及组织中可检测到的与肿瘤相关的物质,达到一定水平时,可反映某些肿瘤的存在。这些肿瘤标志物还能分析病程、监测疗效及复发、判断预后,达到辅助临床改
导言:肿瘤标志物在1978年就被发现了,它是指在血液、体液及组织中可检测到的与肿瘤相关的物质,达到一定水平时,可反映某些肿瘤的存在。这些肿瘤标志物还能分析病程、监测疗效及复发、判断预后,达到辅助临床改善对患者进一步处理的目的。最近发表在《自然》杂志上的一项研究表明,TMBIM6基因可以作为几种癌症疾病预后的预测生物标志物。

TMBIM6是内质网(ER)应激的抑制剂,最初命名为BAX抑制剂(BI)-12。BI-1/TMBIM6是含蛋白3家族跨膜BI-1基序的成员。TMBIM6是一种钙离子通道样蛋白,可降低内质网ER膜表面表达的钙离子稳态。它在许多癌症类型中上调,包括乳腺癌、肺癌、前列腺癌、鼻咽癌和肝癌。
在之前的研究中,TMBIM6的过度表达通过调节细胞的流动性和侵袭性以及葡萄糖代谢来促进肿瘤转移。抑制TMBIM6会导致细胞死亡,从而减少肿瘤的发生。最近,研究人员报道了Sp1和PKC调节TMBIM68的转录表达。PKC在各种癌症类型中也有高表达,如在肝癌、前列腺癌和乳腺癌中。尽管许多证据支持TMBIM6参与了多种癌症的发生,但TMBIM6在癌症进展中作用的分子机制研究较少。
雷帕霉素(mTOR)的机械靶点在细胞代谢、细胞生长和营养敏感方面起着关键作用。mTOR复合物(mTORC)1和mTORC2是两种结构和功能不同的蛋白质复合物,在癌症和糖尿病中经常过度表达。
在本研究中,研究人员确定TMBIM6是mTORC2在ER膜上的主要结合伙伴。这样的结果为调控AKT的激活和肿瘤发生的mTORC2–TMBIM6核糖体轴提供了证据。
为了研究TMBIM6在肿瘤进展中的致癌作用,研究人员首先分析了来自NCBI/GEO的多个肿瘤样本的TMBIM6 mRNA表达谱数据集。这些分析显示,TMBIM6在纤维肉瘤、宫颈癌、子宫内膜癌和外阴癌、乳腺癌、肺癌和前列腺癌中显著过度表达。接下来,研究人员用组织微阵列比较了TMBIM6在同一肿瘤组织中的表达水平,也得到了相似的结果。
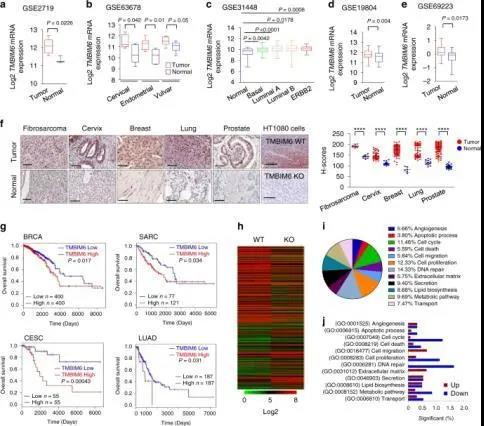
肿瘤组织中TMBIM6表达增加
该研究发现,TMBIM6缺失或敲除会抑制原发肿瘤的生长。此外,mTORC2的激活被TMBIM6上调,并刺激糖酵解、蛋白质合成、脂质合成基因和糖基化蛋白的表达。此外,研究人员发现BIA化合物,一种潜在的TMBIM6拮抗剂,可以阻止TMBIM6与mTORC2结合,降低mTORC2活性,还可以调节TMBIM6泄漏的钙离子,进一步抑制肿瘤的形成和进展。
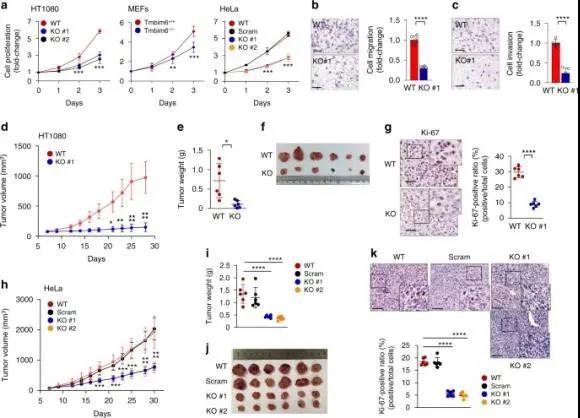
TMBIM6促进肿瘤生长。
TMBIM6通过mTORC2核糖体轴激活AKT通路,评价调节WT细胞和TMBIM6-KO-HT1080细胞肿瘤进展的信号蛋白分子。
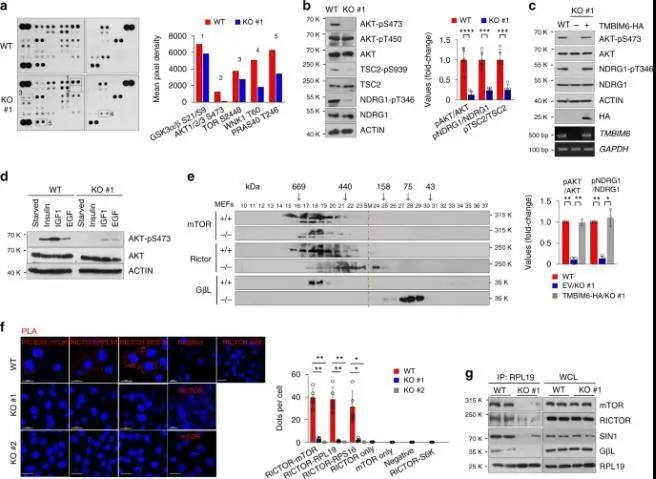
TMBIM6调节mTORC2的激活
本研究结果显示,TMBIM6通过直接结合和刺激钙离子释放来增强mTORC2的活性和组装。TMBIM6的破坏限制了原发性肿瘤的生长,并损害了癌细胞的新陈代谢。此外,研究人员还发现小分子化合物BIA是一种潜在的抗癌药物,可以阻止mTORC2和TMBIM6之间的结合。
该研究表明,TMBIM6通过调节糖酵解和PPP来调节糖代谢,这对mTORC2的活性和信号传递至关重要。鉴于在乳腺癌、前列腺癌、宫颈癌和肺癌中观察到的TMBIM6上调,由mTORC2介导的代谢变化,尤其是AKT可能是癌症进展的主要机制。此外,TMBIM6缺失抑制GSH的生物合成,GSH可能更容易受到活性氧和脂质生物合成的影响,从而抑制肿瘤的发生。本研究表明,TMBIM6是调节mTORC2活性和肿瘤细胞生物能量的重要调节因子。
这些数据表明,TMBIM6作为几种癌症疾病预后的预测生物标志物具有潜在的临床价值。
原始出处:
Hyun-Kyoung Kim, Kashi Raj Bhattarai, Raghu Patil Junjappa, et.al. TMBIM6/BI-1 contributes to cancer progression through assembly with mTORC2 and AKT activation. Nature Communications 11 August 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#COMMUN#
55
#Nat#
0
#TMB#
61
#原发性#
50
#原发性肿瘤#
57
👍🏻
96