JAHA:青少年颈动脉内膜中层厚度进展的预测因素
2021-09-07 MedSci原创 MedSci原创
收缩压、动脉高血压、低密度和非高密度脂蛋白胆固醇以及丙氨酸转氨酶可预测青少年cIMT的进展,尽管危险因素水平主要在既定的参考范围内。
心血管疾病取决于危险因素暴露的持续时间和时间进程。先前关于年轻人颈动脉内膜中层厚度(cIMT)进展的危险因素的报告大多仅限于高危或易受某些类型偏倚影响的人群。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员旨在根据一般人群颈动脉的重复超声评估来揭示早期血管病理学的危险因素特征。
 研究人员从平均年龄为15.8±0.9岁的普通人群中抽取了956名青少年,并评估了危险因素,其中56.2%为女性。在基线和平均22.5±3.4个月后通过高分辨率超声测量了受试者cIMT。研究人员使用线性混合模型对潜在混杂因素进行多变量调整,并探究基线险因素对cIMT进展的影响。
研究人员从平均年龄为15.8±0.9岁的普通人群中抽取了956名青少年,并评估了危险因素,其中56.2%为女性。在基线和平均22.5±3.4个月后通过高分辨率超声测量了受试者cIMT。研究人员使用线性混合模型对潜在混杂因素进行多变量调整,并探究基线险因素对cIMT进展的影响。
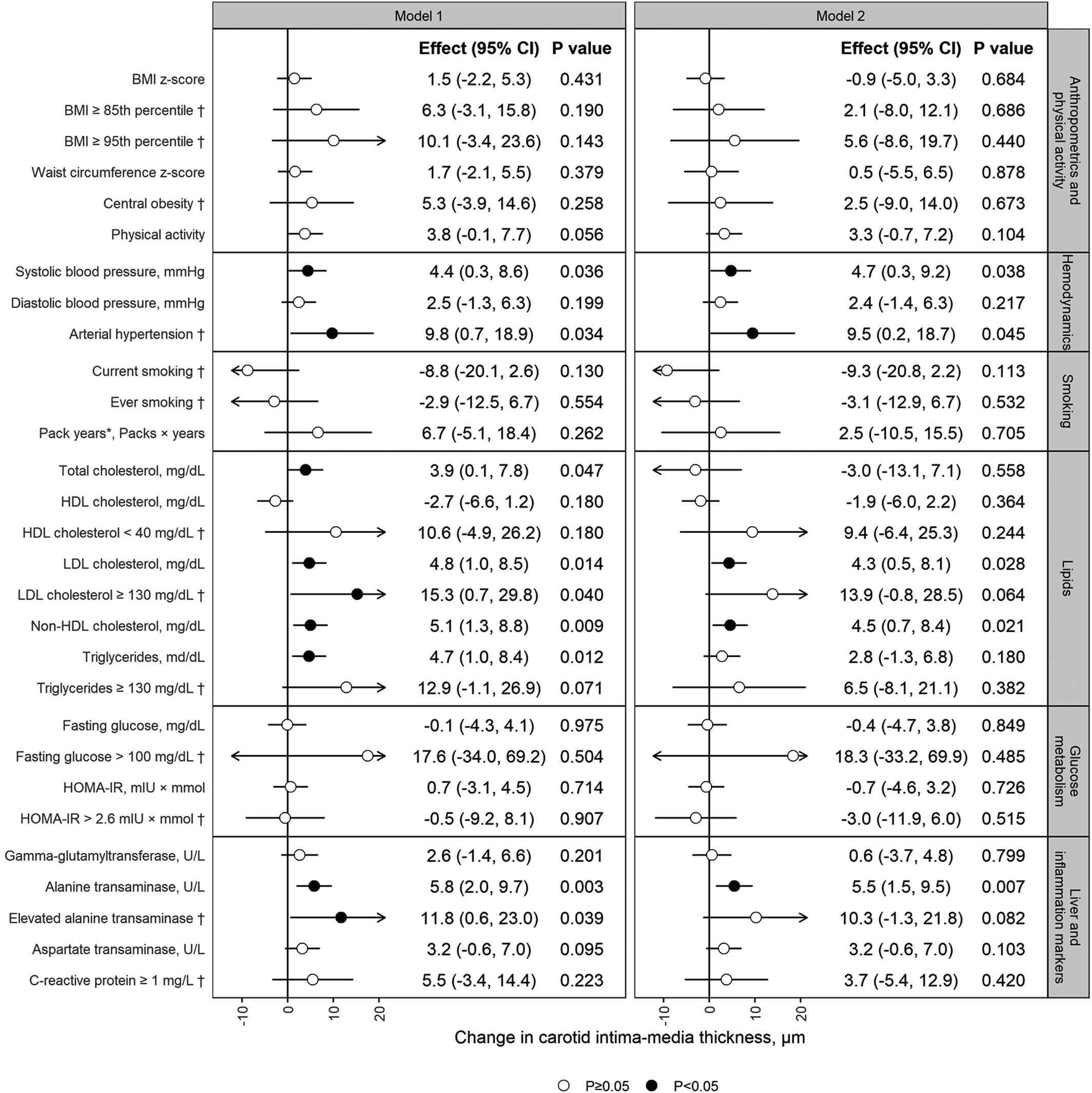 研究人员发现对于丙氨酸转氨酶(5.5μm;95%CI为1.5–9.5)、收缩压(4.7μm;0.3–9.2)、动脉高血压(9.5μm,0.2–18.7)和非高密度脂蛋白胆固醇(4.5μm;0.7–8.4)和低密度脂蛋白胆固醇(4.3微米;0.5–8.1),可得到与cIMT进展之间显著的相关性。
研究人员发现对于丙氨酸转氨酶(5.5μm;95%CI为1.5–9.5)、收缩压(4.7μm;0.3–9.2)、动脉高血压(9.5μm,0.2–18.7)和非高密度脂蛋白胆固醇(4.5μm;0.7–8.4)和低密度脂蛋白胆固醇(4.3微米;0.5–8.1),可得到与cIMT进展之间显著的相关性。
由此可见,收缩压、动脉高血压、低密度和非高密度脂蛋白胆固醇以及丙氨酸转氨酶可预测青少年cIMT的进展,尽管危险因素水平主要在既定的参考范围内。这些结果再次强调了生命早期就开始预防的必要性,这些结果挑战了当前指南建议的对高危青少年的关注重点。
原始出处:
Sophia J. Kiechl.et al.Predictors of Carotid Intima‐Media Thickness Progression in Adolescents—The EVA‐Tyrol Study.JAHA.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.120.020233
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#内膜#
74
#颈动脉#
64
#预测因素#
60
#AHA#
59
#颈动脉内膜中层厚度#
73