JCO:输精管切除术与前列腺癌有关?
2014-07-24 何Jason 医学专业新闻
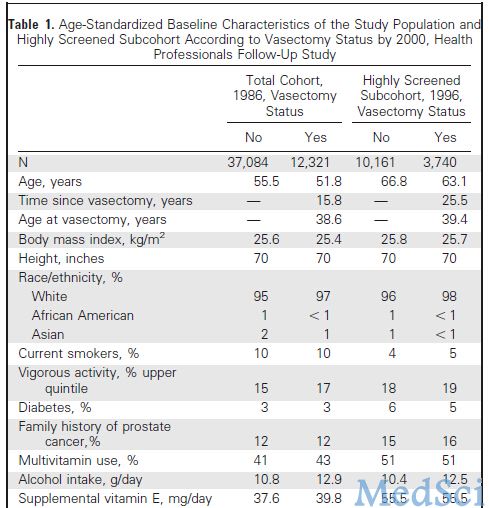
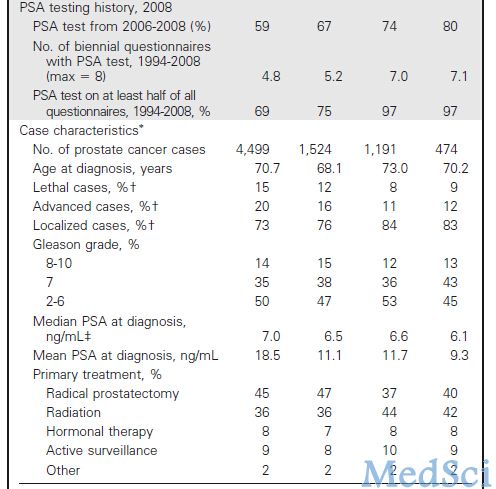
在线发表于《临床肿瘤学杂志》(JCO)的一项队列研究显示,对于接受了输精管切除术的男性人群,前列腺癌风险将出现增加。该研究共纳入超过50,000个样本。总体而言,输精管切除术与前列腺癌风险增加10%有关,与高度恶性和致死性前列腺癌风险增加20%有关。常规接受PSA筛查的男性群体,该风险甚至增加50%。研究的主要作者,来自哈佛大学公共卫生学院的Lorelei A. Mucci, ScD强调,前列腺癌
在线发表于《临床肿瘤学杂志》(JCO)的一项队列研究显示,对于接受了输精管切除术的男性人群,前列腺癌风险将出现增加。该研究共纳入超过50,000个样本。
总体而言,输精管切除术与前列腺癌风险增加10%有关,与高度恶性和致死性前列腺癌风险增加20%有关。常规接受PSA筛查的男性群体,该风险甚至增加50%。
研究的主要作者,来自哈佛大学公共卫生学院的Lorelei A. Mucci, ScD强调,前列腺癌风险的增加是“较小的”。他说:“随访24年间,致死性前列腺癌的累计发病率增加了1.6%。因此,医生在决定进行输精管切除术之前,应充分权衡利弊。”
Stephen说:“我们对于接受相关手术的患者,应进行严密的监测。但这项研究并不足以改变我们的治疗模式。”
关于输精管切除术与前列腺癌之间的联系,目前仍存在很大争议。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JCO#
62
#输精管#
66
#切除术#
105
#输精管切除术#
78