Circulation:重度主动脉瓣狭窄合并二尖瓣狭窄的患者,经主动脉置换术后的存活情况
2019-10-08 MedSci MedSci原创
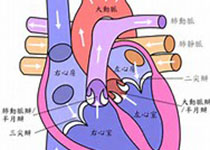
重度主动脉瓣狭窄患者常合并二尖瓣狭窄常。在主动脉瓣狭窄合并二尖瓣狭窄的情况下,评估二尖瓣狭窄的严重程度具有挑战性,因为两个病变瓣膜之间存在血流动力学的相互作用。主动脉瓣置换术(AVR)治疗重度主动脉瓣狭窄对二尖瓣狭窄的影响尚不清楚。本研究旨在评估AVR对二尖瓣狭窄血流动力学的影响,以及有无二尖瓣狭窄的重度主动脉瓣狭窄患者的临床疗效。研究人员回顾性调查了2008年-2015年因重度主动脉瓣狭窄行AV
重度主动脉瓣狭窄患者常合并二尖瓣狭窄常。在主动脉瓣狭窄合并二尖瓣狭窄的情况下,评估二尖瓣狭窄的严重程度具有挑战性,因为两个病变瓣膜之间存在血流动力学的相互作用。主动脉瓣置换术(AVR)治疗重度主动脉瓣狭窄对二尖瓣狭窄的影响尚不清楚。本研究旨在评估AVR对二尖瓣狭窄血流动力学的影响,以及有无二尖瓣狭窄的重度主动脉瓣狭窄患者的临床疗效。
研究人员回顾性调查了2008年-2015年因重度主动脉瓣狭窄行AVR或经导管AVR治疗的患者。多普勒超声心动图显示二尖瓣平均梯度≥4mm Hg为二尖瓣狭窄;根据二尖瓣面积(>2.0 cm2或≤2.0 cm2)对患者进行分层。评估二尖瓣狭窄患者AVR前后的MVA。
在190位重度主动脉瓣狭窄合并二尖瓣狭窄的患者(76±9岁,42%为男性)中,184位与362位无二尖瓣狭窄的重度主动脉瓣狭窄患者相匹配。在所有二尖瓣狭窄的患者中,AVR术后MVA平均增加了0.26±0.59 cm2(从2.00±0.50增加到2.26±0.62 cm2, P<0.01)。105位(55%)患者的MVA有增加,34位(18%)患者的保持不变。每搏输出量≤45 mL/m2和经导管AVR是术后MVA增加的独立相关因素。在107位二尖瓣显著狭窄(MVA≤2.0 cm2)的患者中,有52位(49%)患者AVR术后MVA增加2cm2以上。中位随访2.9年时间内,真正的二尖瓣狭窄是全因死亡的独立预测因素(校正风险比1.88,95% CI 1.20-2.94;P<0.01)。
近一半的重度主动脉瓣狭窄合并二尖瓣狭窄的患者在AVR术后MVA获得改善。同时近一半的重度主动脉瓣狭窄合并二尖瓣狭窄的患者在AVR术后MVA仍不超过≤2.0 cm2(真正的二尖瓣狭窄),而真正的二尖瓣狭窄与重度主动脉瓣狭窄患者AVR术后的存活率较低有关。
原始出处:
Nahoko Kato, et al.Hemodynamics and Prognostic Impact of Concomitant Mitral Stenosis in Patients Undergoing Surgical or Transcatheter Aortic Valve Replacement for Aortic Stenosis.Circulation. 2019;140:1251–1260
本文系梅斯医学(MedSci)原创编译,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#二尖瓣狭窄#
85
#重度主动脉瓣狭窄#
74
#置换#
67
#主动脉瓣#
71
#主动脉#
56
#二尖瓣#
61
#置换术#
59