Ponesimod治疗复发性多发性硬化症的III期研究结果:符合其主要和次要终点
2019-07-26 Allan MedSci原创
Ponesimod是一种选择性鞘氨醇-1-磷酸受体1(S1P1)调节剂,Ponesimod被认为能够抑制S1P1活性并减少循环淋巴细胞的数量。强生公司近日公布了III期OPTIMUM研究的正面结果,该研究评估了Ponesimod治疗复发性多发性硬化症的有效性和安全性。
Ponesimod是一种选择性鞘氨醇-1-磷酸受体1(S1P1)调节剂,Ponesimod被认为能够抑制S1P1活性并减少循环淋巴细胞的数量。强生公司近日公布了III期OPTIMUM研究的正面结果,该研究评估了Ponesimod治疗复发性多发性硬化症的有效性和安全性。OPTIMUM的主要终点是直至研究结束时的年复发率(ARR),关键的次要终点是疲劳相关症状从基线到第108周的变化。结果显示,该研究符合其主要和次要终点。
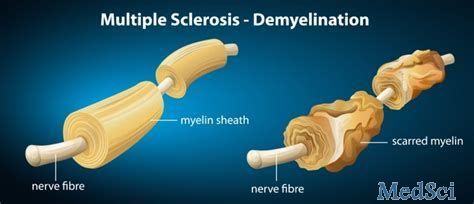
多发性硬化症是一种脱髓鞘性神经病变,患者脑或脊髓中的神经细胞表面的绝缘物质(即髓鞘)受到破坏,神经系统的信号转导受损,导致一系列可能发生的症状,影响患者的活动、心智、甚至精神状态。
原始出处:
http://www.firstwordpharma.com/node/1655203#axzz5ug3cIKrI
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#多发性#
58
#研究结果#
64
#III期研究#
50
#硬化症#
66
#复发性#
62
#复发性多发性硬化症#
70
#III#
66
#ESI#
54
#III期#
53
#Ponesimod#
74