JAMA子刊:任何年龄确诊抑郁症都与痴呆症风险上升有关!
2023-09-01 中国全科医学杂志 中国全科医学杂志 发表于上海
无论是在早年、中年或晚年诊断出抑郁症,都与痴呆症风险上升有关。抑郁症患者患痴呆症的风险都要增加100%以上,且男性风险高于女性。
JAMA Neurology杂志近期发表一篇文章,来自丹麦奥胡斯大学的Holly Elser及其研究团队利用超过140万丹麦成年人随访数据,评估了不同年龄段确诊抑郁症与痴呆症风险之间的关系。结果显示,无论是在早年、中年或晚年诊断出抑郁症,都与痴呆症风险上升有关。抑郁症患者患痴呆症的风险都要增加100%以上,且男性风险高于女性。

分析结果显示
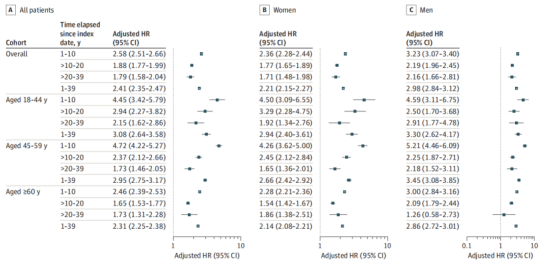
与对照组相比,抑郁症患者患痴呆症的累计发生率增加,整体风险是对照组的2.41倍,无论分组如何,抑郁症患者的痴呆症风险都增加1倍以上。即使经过20年、30年,甚至39年,依然可以观察到确诊抑郁症与痴呆症风险之间的关联(HR 1.79;95% Cl,1.58-2.04)。
根据年龄进行分组
早年确诊抑郁症与痴呆症风险增加208%有关,中年确诊抑郁症与痴呆症风险增加195%有关,老年确诊抑郁症与痴呆症风险增加131%有关。
根据性别进行分组
抑郁症男性比女性患痴呆症的风险更高。男性确诊抑郁症与痴呆症风险增加198%有关,女性确诊抑郁症与痴呆症风险增加121%有关。
在确诊抑郁症前后6个月的时间内,接受抗抑郁药物治疗与痴呆症风险无关(接受治疗HR 2.42 vs 未接受治疗HR 2.35)。但是与1次住院就诊的患者相比,多次住院就诊与痴呆症风险进一步增加有关(2次住院HR 1.33,3次住院HR 1.62,≥4次HR 1.49)。
研究结果提示,抑郁症不仅是痴呆症的早期症状,还与痴呆症风险增加有关。
Abstract
Association of Early-, Middle-, and Late-Life Depression With Incident Dementia in a Danish Cohort
Importance: Late-life depressive symptoms are associated with subsequent dementia diagnosis and may be an early symptom or response to preclinical disease. Evaluating associations with early- and middle-life depression will help clarify whether depression influences dementia risk.
Objective: To examine associations of early-, middle-, and late-life depression with incident dementia.
Design, setting, and participants: This was a nationwide, population-based, cohort study conducted from April 2020 to March 2023. Participants included Danish citizens from the general population with depression diagnoses who were matched by sex and birth year to individuals with no depression diagnosis. Participants were followed up from 1977 to 2018. Excluded from analyses were individuals followed for less than 1 year, those younger than 18 years, or those with baseline dementia.
Exposure: Depression was defined using diagnostic codes from the International Classification of Diseases (ICD) within the Danish National Patient Registry (DNPR) and Danish Psychiatric Central Research Register (DPCRR).
Main outcomes and measure: Incident dementia was defined using ICD diagnostic codes within the DPCRR and DNPR. Cox proportional hazards regression was used to examine associations between depression and dementia adjusting for education, income, cardiovascular disease, chronic obstructive pulmonary disease, diabetes, anxiety disorders, stress disorders, substance use disorders, and bipolar disorder. Analyses were stratified by age at depression diagnosis, years since index date, and sex.
Results: There were 246 499 individuals (median [IQR] age, 50.8 [34.7-70.7] years; 159 421 women [64.7%]) with diagnosed depression and 1 190 302 individuals (median [IQR] age, 50.4 [34.6-70.0] years; 768 876 women [64.6%]) without depression. Approximately two-thirds of those diagnosed with depression were diagnosed before the age of 60 years (684 974 [67.7%]). The hazard of dementia among those diagnosed with depression was 2.41 times that of the comparison cohort (95% CI, 2.35-2.47). This association persisted when the time elapsed from the index date was longer than 20 to 39 years (hazard ratio [HR], 1.79; 95% CI, 1.58-2.04) and among those diagnosed with depression in early, middle, or late life (18-44 years: HR, 3.08; 95% CI, 2.64-3.58; 45-59 years: HR, 2.95; 95% CI, 2.75-3.17; ≥60 years: HR, 2.31; 95% CI, 2.25-2.38). The overall HR was greater for men (HR, 2.98; 95% CI, 2.84-3.12) than for women (HR, 2.21; 95% CI, 2.15-2.27).
Conclusions and relevance: Results suggest that the risk of dementia was more than doubled for both men and women with diagnosed depression. The persistent association between dementia and depression diagnosed in early and middle life suggests that depression may increase dementia risk.
文章来源:Elser H, Horváth-Puhó E, Gradus J L, et al. Association of Early-, Middle-, and Late-Life Depression With Incident Dementia in a Danish Cohort[J]. JAMA neurology, 2023.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












