Lancet oncol:右结肠癌切除术该不该清扫中央区淋巴结?
2021-02-16 Nebula MedSci原创
右结肠癌行淋巴结清扫术是否会增加围手术期并发症或提高生存率仍有争议。本试验旨在对比腹腔镜右半结肠切除术中完全结肠系膜切除(CME)与D2分离治疗右半结肠癌患者的疗效和安全性。本文报道了该试验的早期安全
右结肠癌行淋巴结清扫术是否会增加围手术期并发症或提高生存率仍有争议。本试验旨在对比腹腔镜右半结肠切除术中完全结肠系膜切除(CME)与D2分离治疗右半结肠癌患者的疗效和安全性。本文报道了该试验的早期安全性结果。
这是一项在中国9个省17家医院开展的一项随机对照3期优势性试验,招募18-75岁的组织学确诊的未发现转移的原发性右半结肠癌(盲肠和横结肠右三分之一之间)患者。在腹腔镜右结肠切除术中,患者随机(1:1)接受CME(包括中央区淋巴结)或D2(不包括中央区淋巴结)处理。主要终点是3年无病存活率。
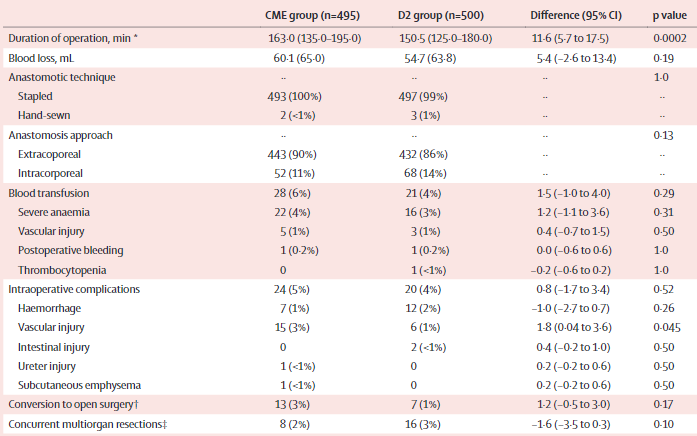
2016年1月11日-2019年12月26日,共招募了1072位患者,排除了77位后,995位被纳入校正意向治疗人群(495位在CME组、500位在D2分离组)。
两组预后情况
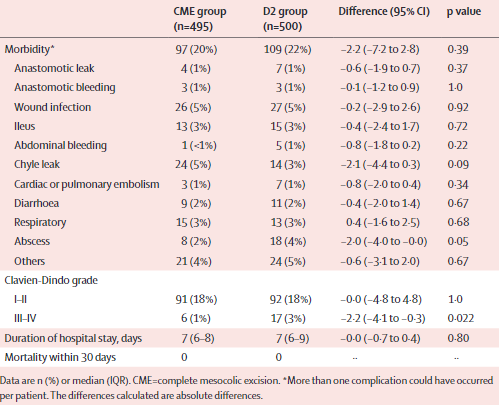
CME组和D2组的手术并发症发生率分别为20%和22%(差异 -2.2%;p=0.39);两组间Clavien-Dindo I-II级并发症发生率相似(均为18%),但CME组的Clavien-Dindo III-IV级并发症发生率明显低于D2组(1% vs 3%;p=0.022);两组均无死亡病例。
两组术后30天内的并发症和死亡率
在术中并发症中,CME组血管损伤明显多于D2组(3% vs 1%;p=0.045)。在CME组进行中央区淋巴结清扫的394位患者中有13位(3%)检出中央区淋巴结转移;无患者存在孤立性的中央区淋巴结转移。
综上,虽然CME手术可能会增加术中血管损伤的风险,但对于有经验的外科医生来说,它通常是安全可行的。
原始出处:
Lai Xu, et al. Short-term outcomes of complete mesocolic excision versus D2 dissection in patients undergoing laparoscopic colectomy for right colon cancer (RELARC): a randomised, controlled, phase 3, superiority trial. The Lancet Oncology. February 12, 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
90
#Lancet#
64
#切除术#
63
有收获
97
#淋巴结#
91
顶刊就是不一样,质量很高,内容精彩!学到很多
78
谢谢梅斯分享这么多精彩信息
98