Opdivo/Yervoy组合显著提高去势抵抗性前列腺癌患者响应率
2019-02-18 不详 MedSci原创
BMS公布了其关键临床试验CheckMate-650的结果,该试验显示Opdivo与Yervoy联合使用显著提高对转移性去势抵抗性前列腺癌患者的响应率。
BMS公布了其关键临床试验CheckMate-650的结果,该试验显示Opdivo与Yervoy联合使用显著提高转移性去势抵抗性前列腺癌患者的响应率。
在第二代激素治疗且未进行化疗的32例患者中,Opdivo与Yervoy联合的客观响应率(ORR)为25%。在基于紫杉烷的化疗后疾病进展的30例患者中,ORR为10%。
在这两组实验中,部分患者中可以观察到明显提高的反应率,包括具有高肿瘤突变负荷的患者和具有同源重组缺陷的患者。
"这项研究的临床结果令人鼓舞,并为更大的患者群体中的联合策略提供了基础。"
Opdivo是一种程序性死亡-1(PD-1)免疫检查点抑制剂,旨在特异性地调控自身免疫系统以恢复抗肿瘤免疫反应。
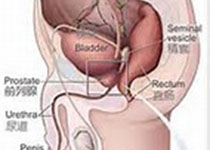
前列腺癌是男性第二位最常见癌症,2018年全球新诊断出近128万病例。与早期前列腺癌不同的是,去势抵抗性前列腺癌(CRPC)即使体内睾酮的量降低,癌症仍然继续增长。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#抗性#
73
#Opdivo#
77
#去势抵抗性前列腺癌#
81
#Yervoy#
83
学习了,涨知识了!
96