Medical Image Analysis: 深度学习预测COVID-19恶性进展
2021-05-13 MedSci原创 MedSci原创
2020年以来,新冠肺炎对人民生活产生了根本性影响。截至2020年8月12日,全球COVID-19感染人数飙升至2020万人(20,162,474),死亡率为3.7% (737,417/20,162,
2020年以来,新冠肺炎对人民生活产生了根本性影响。截至2020年8月12日,全球COVID-19感染人数飙升至2020万人(20,162,474),死亡率为3.7% (737,417/20,162,474),给公共医疗体系带来巨大挑战。法国和英国的死亡率居世界首位,分别为15.8%(30227 / 191265)和14.9%(46,526/312,793)。相比之下,其他一些国家的死亡率要低得多,如德国4.2% (9,207/218,519)。
由于COVID-19具有高度传染性,因此许多患者可以同时涌入医院进行诊断和治疗,这极大地挑战了公共医疗系统。通常根据首次评估的症状严重程度确定治疗优先级。但是,临床观察表明,某些症状较轻的患者可能会迅速恶化。因此,确定患者早期恶化以优化治疗策略至关重要。
CongFang等的研究主要集中于利用入院时确定的临床变量或定量CT参数,通过多元回归光梯度增压机(LightGBM) 或LASSO进行进展预测。然而,这些方法的性能与实际使用相比仍有很大差距,原因有三:1)需要人工对特征模式进行量化,导致分析前信息丢失;2)时间线索或多或少被忽略,但对准确预测至关重要;3)胸部CT扫描与临床数据采集的患者特征不同,但两者之间的互补性没有充分发挥作用。

为解决上述问题,该团队借助人工智能(AI)技术,提供了预测COVID-19恶性进展的准确模型。基于深度学习方法,该模型有效挖掘了胸部CT扫描静态临床数据和动态序列中的互补信息。它以端到端方式对原始数据进行操作,这意味着不需要任何特征模式的手工设计或临床医生的干预。此外,该模型自动识别导致恶性进展的关键指标,包括肌钙蛋白、脑利钠肽、白细胞计数、天冬氨酸转氨酶、肌酐和超敏c反应蛋白。

本系统预测COVID-19恶性进展的流程。首先,3D ResNet和MLP分别对胸部CT扫描和临床数据进行编码。然后,我们将这两个特征结合起来,并将它们输入一个LSTM来建模时间信息。最后,利用几个全连通层进行预测。
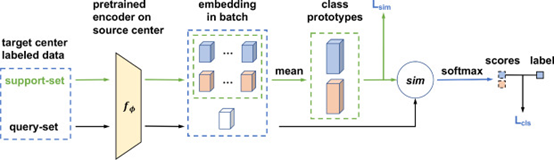
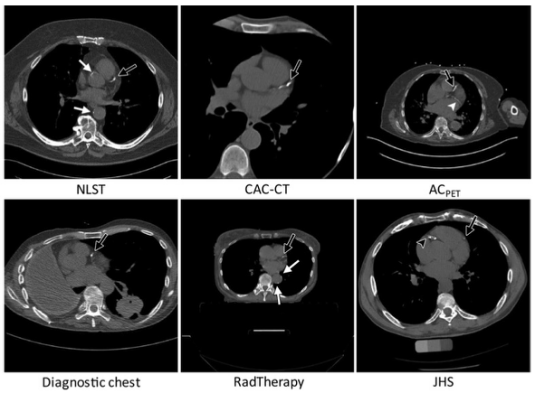
多中心域自适应过程。首先,我们在源中心对编码器进行预训练,然后,通过基于度量的方法对模型进行调整,将从源中心学习到的原型表示传递给目标中心。
我们的工作构建了COVID-19恶性进展的早期预警系统,以减少患者分层不确定性,优化诊断和治疗,提高医疗资源配置效率,提高医疗系统应急响应能力。最终降低死亡率。对三个队列的综合实验表明,我们的系统同时使用CT扫描和临床数据,在内部验证(受试者工作特征曲线下面积: 0.920, 95%置信区间:[0.861, 0.979],队列1),但更重要的是,在外部验证中具有强大的泛化能力(AUC: 0.885, 95% CI:[0.847, 0.923],队列2;AUC: 0.862, 95% CI:[0.789, 0.935],第三组)。

比较不同方法对队列的ROC曲线
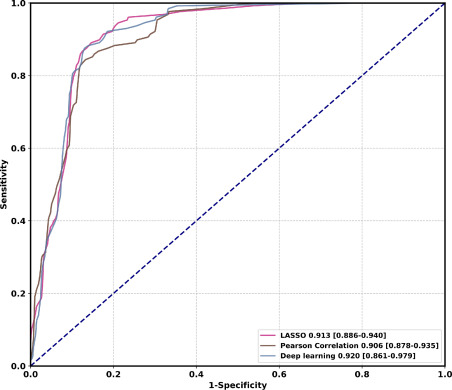
比较不同特征选择算法在队列上的ROC曲线
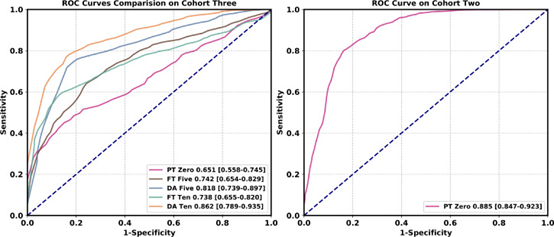
多中心研究中不同方法的ROC曲线比较。在每个类中,在域适应过程中使用相同数量的样本。
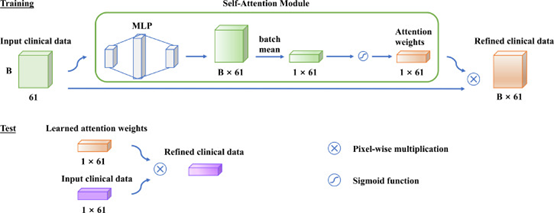
预后因素的自我注意模块。B × 61表示批次大小和向量长度。
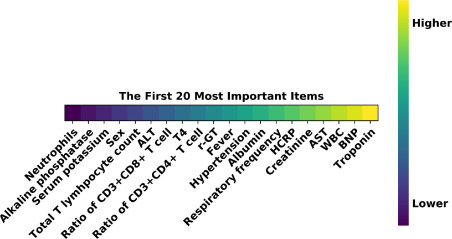
临床资料中最重要的预后因素。
冠状病毒引起的肺炎给公共医疗系统带来巨大压力。这些患者如果没有及时有效的治疗,最终会发展为多器官衰竭并伴有高死亡率。因此,对症状轻且恶性进展至重/危重期风险高的患者进行早期预测和早期积极治疗是降低死亡率的重要途径。
该研究团队开发的这种具有深度学习技术的预警系统,可用于预测COVID-19恶性进展。利用CT扫描和门诊患者的临床数据,在单中心研究中AUC0.920。还提出了一种领域自适应方法,以改善模型的通用性并在多中心研究中实现平均AUC达0.874。此外,该模型自动识别导致恶性进展的关键指标,包括肌钙蛋白、脑利钠肽、白细胞计数、天冬氨酸转氨酶、肌酐和超敏c反应蛋白。
综上所述,该预警系统以深度学习技术为基础,结合CT序列扫描和临床数据,能够准确预测COVID-19恶性进展。与传统的机器学习方法相比,基于深度学习的方法可以学习具有区别性的特征模式,并显著提高预测性能。在多中心研究中,通过域自适应,提高了该方法的泛化能力。该研究提出的方法通过一种廉价、广泛可用的即时检测来识别潜在严重、危险预后的 COVID-19患者。该系统可以部署在降低COVID-19死亡率的前线。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ANA#
49
#Anal#
64
#DIC#
58
学习
80
#Medical#
96
#Med#
0