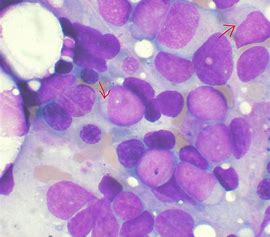
Leukemia:LSD1有望称为治愈MDS相关白血病的靶点!
2018-01-15 MedSci MedSci原创
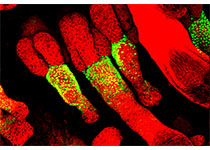
NCD38能对异常情况下被LSD1沉默的造血调节因子的超强启动子去抑制,从而延迟白血病进程,发挥抗白血病的作用,抑制MDS相关白血病的不良预后。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#MDS#
59
#MDS相关白血病#
73
学习了谢谢分享!!
102
#LSD1#
84
学习了谢谢分享!!
104