
载脂蛋白E4(APOE ε4)等位基因是晚发性阿尔茨海默病(AD)的主要遗传风险因素。然而,即使在年龄大于90岁的APOE ε4携带者中2,也不是所有APOE ε4携带者都会发生痴呆。一个潜在的媒介可能是C 反应蛋白(CRP)。
血液中CRP的升高只与APOE ε4等位基因携带者的AD风险增加有关,这表明CRP可能改变APOE ε4的作用,导致与AD相关的神经变性。尽管如此,APOE ε4和CRP对认知能力下降和AD病理的相互作用仍是未知的。
CRP是一种参与对毒素或伤害的免疫反应的蛋白质,在系统性炎症中,CRP水平随年龄增长而增加。CRP有两种类型:1)原生CRP(pCRP)是一种五聚体低聚蛋白和急性期反应物,在活跃的炎症反应中产生;2)单体CRP(mCRP),或pCRP的游离亚单位,在急性期和之后由pCRP的不可逆解离产生,它的水溶性更低,受损组织。CRP被认为与衰老相关的慢性疾病的发病机制有关,包括心血管疾病、老年性黄斑变性和中风后炎症。
藉此,波士顿大学医学院的Qiushan Tao等人,利用阿尔茨海默病神经成像倡议(ADNI)队列,探究了APOE ε4状态(无、一个和两个APOE ε4等位基因)和外周CRP对认知和体内AD生物标志物的独立和交互影响,包括脑脊液(CSF)淀粉样β肽42(Aβ42)、总tau(t-Tau)和磷酸化tau(p-Tau)。
他们分析了阿尔茨海默病神经影像倡议(ADNI)研究的数据,包括APOE基因型;血浆CRP浓度;诊断状态(即。MCI和AD导致的痴呆);迷你精神状态检查(MMSE)和临床痴呆评分(CDR)痴呆分期工具;脑脊液(CSF)中淀粉样β肽(Aβ42)、总tau(t-tau)和磷酸化tau(p-tau)的浓度;和淀粉样(AV45)PET成像。多变量回归分析检验了血浆CRP和APOE与认知和生物标志物结果之间的关联。
在566名ADNI参与者中,274人(48.4%)没有,222人(39.2%)有一个,70人(12.4%)有两个APOEε4等位基因。
只有在有两个APOE ε4等位基因的参与者中,CRP升高与基线和12个月随访的MMSE降低有关。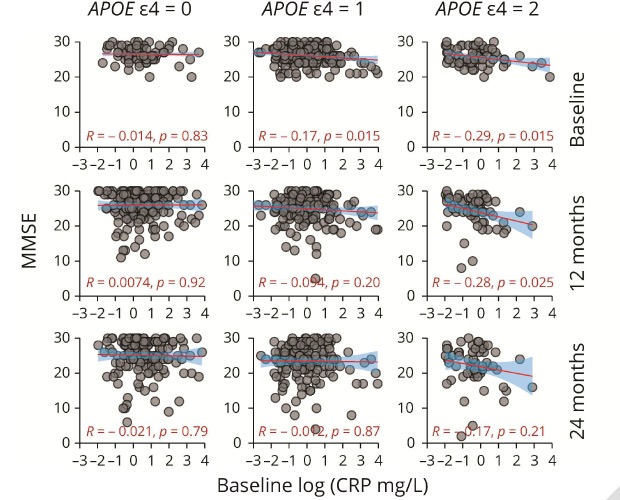
两个APOE ε4等位基因和血浆CRP升高的交互作用与CSF中t-Tau(β = 11.21, SE = 3.37, p < 0.001)和p-Tau(β = +2.74, SE = 1.14, p < 0.01)水平的升高有关。在没有APOE ε4等位基因的人中,CRP的升高与CSF t-Tau和p-Tau的降低有关。这些影响在12个月的随访中更为强烈。
这个研究的重要意义在于:外周炎症期间释放的CRP可能是APOE ε4相关的AD神经退行性的介体,可作为AD的药物靶点。
原文出处:
Tao Q, Alvin Ang TF, Akhter-Khan SC, Itchapurapu IS, Killiany R, Zhang X, Budson AE, Turk KW, Goldstein L, Mez J, Alosco ML, Qiu WQ; Alzheimer’s Disease Neuroimaging Initiative. Impact of C-Reactive Protein on Cognition and Alzheimer Disease Biomarkers in Homozygous Apolipoprotein E ɛ4 Carriers. Neurology. 2021 Jul 15:10.1212/WNL.0000000000012512. doi: 10.1212/WNL.0000000000012512. Epub ahead of print. PMID: 34266923.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#神经退行性变#
76
#神经退行#
57
#Neurol#
72
#C反应蛋白#
59
学习一下
83