轻松掌握:甲亢和甲减如何治疗?
2016-07-16 王维波 医学界内分泌频道
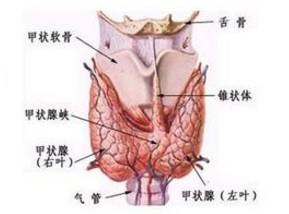
甲状腺虽然小,却是人体非常重要的内分泌器官。它位于甲状软骨下方,气管两旁,很多人认为甲状腺形似蝴蝶,犹如盾甲,故以此命名。甲状腺的主要功能是合成甲状腺激素,调节机体的基础代谢,影响机体的正常生长发育,临床上常见的甲状腺疾病为甲状腺功能亢进(甲亢)和甲状腺功能减退(甲减)。一个是“亢”,一个是“减”,该如何治疗呢?甲亢的治疗:甲亢,是指甲状腺腺体本身功能亢进、合成和分泌甲状腺激素增多,主要临床表现为
甲状腺虽然小,却是人体非常重要的内分泌器官。它位于甲状软骨下方,气管两旁,很多人认为甲状腺形似蝴蝶,犹如盾甲,故以此命名。
甲状腺的主要功能是合成甲状腺激素,调节机体的基础代谢,影响机体的正常生长发育,临床上常见的甲状腺疾病为甲状腺功能亢进(甲亢)和甲状腺功能减退(甲减)。一个是“亢”,一个是“减”,该如何治疗呢?
甲亢的治疗:
甲亢,是指甲状腺腺体本身功能亢进、合成和分泌甲状腺激素增多,主要临床表现为高代谢症状,如烦躁、失眠、乏力多汗等,严重者可出现甲亢危象、昏迷甚至危及生命;也存在少数老年患者高代谢症状不典型,仅表现为乏力、厌食、抑郁、嗜睡、称淡漠型甲亢。

目前甲亢一般治疗包括休息、补充营养热量等,治疗主要包括三种方式即抗甲状腺药物(ATD)、同位素碘(I131)和手术治疗,目前我国主要以药物治疗为主,而国外更多选择I131治疗为主,现比较下三种治疗方法的不同之处。

(甲亢三种治疗方法比较,点击可看大图)
甲减的治疗:
甲减,是指由于甲状腺激素合成和分泌减少、或组织利用不足导致的全身代谢减低综合征。病因主要为自身免疫性损伤、甲状腺破坏、甲状腺激素合成障碍、缺碘或服药某些药物等。
临床上按照甲状腺功能减低的程度分为临床甲减和亚临床甲减。主要表现为畏寒、嗜睡、体重增加、便秘、记忆力减退等,严重者可出现黏液性水肿昏迷等危险情况。

1,亚临床甲减的治疗:
亚临床甲减一般不需治疗,但如果促甲状腺素(TSH)>10mI/UL,结合患者病情,可选择补充甲状腺激素治疗。
2,临床甲减的治疗:
一般需要终身服用补充甲状腺激素的药物。
在早期轻型病例,以口服甲状腺片或左甲状腺素为主;中、晚期重型病例,除口服甲状腺片或左旋甲状腺素外,需对症治疗如给氧、输液、控制感染、控制心力衰竭等。
3,两种临床常用药物——甲状腺片和左甲状腺素钠的不同:

(点击可看大图)
参考文献:
《甲状腺疾病诊治指南》
《妊娠和产后甲状腺疾病诊治指南》
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












文章很好,非常有益
103
学习学习!
138
值得一读
117
文章不错
158
#甲减#
70