JNS:前后联合治疗胸腰段粉碎骨折长期效果好
2014-06-06 佚名 丁香园
胸腰段骨折现代手术治疗的目的在于提供足够的稳定,以防止复位丢失和促进愈合。尽管关于初期稳定的重要性观点一致,但不稳定性胸腰段骨折的最佳手术选择,即后路、前路或前后联合手术,仍存在争论。很多学者主张前后联合手术。【原文下载】 前后联合手术的优点在于提高了初期稳定性,复位效果好及术后复位丢失减少。为重建前柱而使用可延伸钛网,可避免取自体髂骨的相关并发症,生物力学上更优越。目前尚无使用可延伸钛网前
胸腰段骨折现代手术治疗的目的在于提供足够的稳定,以防止复位丢失和促进愈合。尽管关于初期稳定的重要性观点一致,但不稳定性胸腰段骨折的最佳手术选择,即后路、前路或前后联合手术,仍存在争论。很多学者主张前后联合手术。【原文下载】
前后联合手术的优点在于提高了初期稳定性,复位效果好及术后复位丢失减少。为重建前柱而使用可延伸钛网,可避免取自体髂骨的相关并发症,生物力学上更优越。目前尚无使用可延伸钛网前后联合手术治疗胸腰椎不稳骨折的长期随访研究。
德国法兰克福脊柱和神经创伤手术中心的学者进行了一项前瞻性研究,提示前后联合+可延伸钛网可成功治疗胸腰段粉碎骨折,长期随访结果良好,文章于2014年5月发表在JNS上。
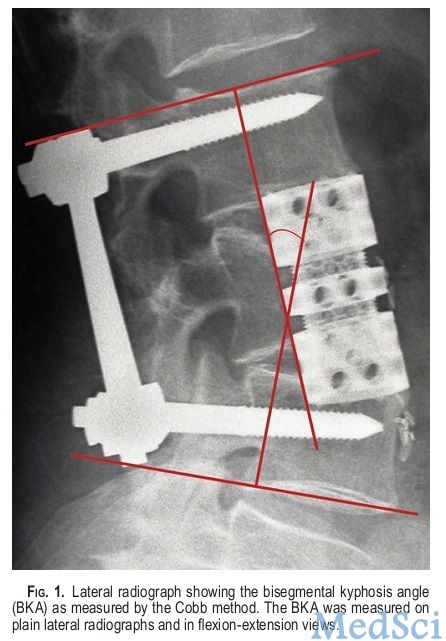
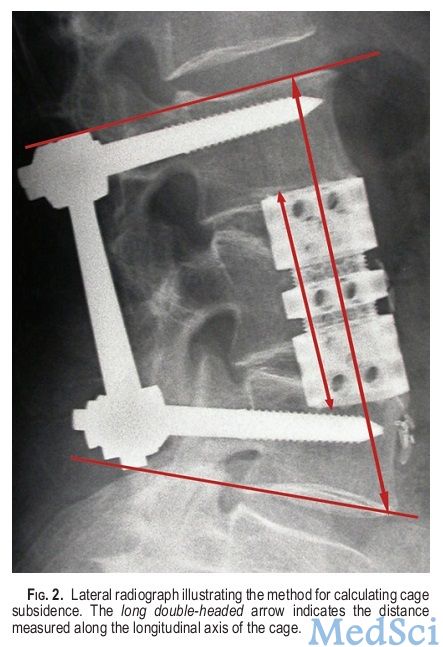
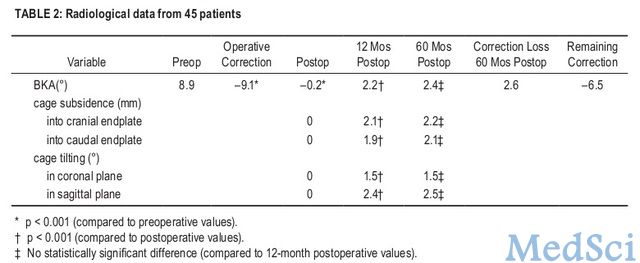
该研究共纳入使用该技术治疗的80例胸腰段骨折(T4-L5)、不稳的连续病例,其骨折AO-Magerl分类为A.3、B或C型,其中45例随访时间达5年,平均年龄44岁。使用该技术,加用或不加用前路钢板。5年随访时,评估病例的X线片(图1,图2,图3)、CT
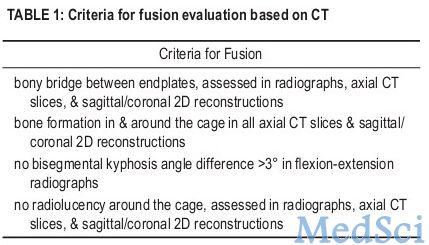
(表1)、Oswestry残障指数、神经功能和临床疗效。

所有病例先行后路USS或USS-II固定,继而行前路骨折椎体次全切除,植入可延伸钛网VBR(局部椎体松质骨填充),L1以上开胸,以下则腹膜外入路。43例由手术医生已经稳定与否,另外前路植入了钢板。
结果显示,开胸相关的并发症发生率高,为26%,无融合器相关并发症。1例因开胸血肿而需翻修手术。术后矫形丢失为由于钛网的轻微下沉而导致,平均为2.4度。动力位片未发现融合器透明线或不稳(表2)。


值得注意的是,本研究中近三分之一的病例存在前路开胸相关的并发症,即使术后5年,依然存在。考虑到此因素,为前后联合手术的缺点,就此而言,单纯后路手术具有优越性。另一方面,本研究中前路手术为开放性开胸手术,若使用胸腔镜技术,将降低开胸带来的并发症。但需要研究加以证实。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








文字生动形象,图片很好
127
#长期效果#
63
#胸腰段#
69
#联合治疗#
59