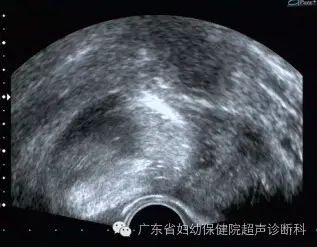
Lancet Oncol:卵巢肿瘤保守治疗的并发症风险真没你想的那么高!
2019-03-13 Jelly 肿瘤资讯
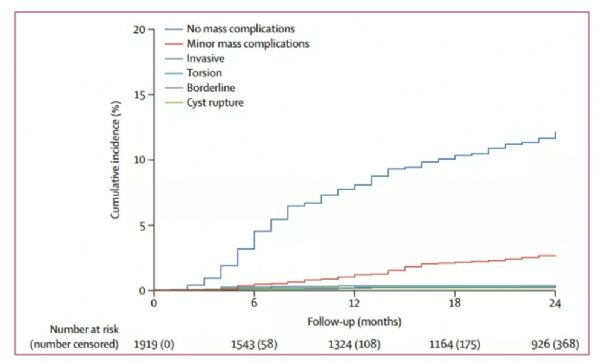
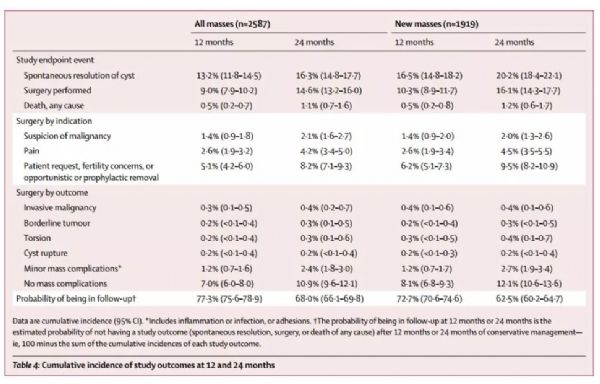
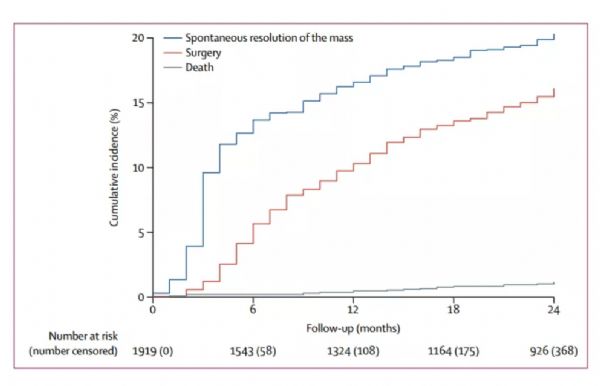
因为可能存在并发症的风险,卵巢肿瘤常通过手术切除。目前对附件包块长期随访的大型前瞻性研究很少。该研究旨在评估附件包块经超声诊断为良性后,随访2年内囊肿并发症和恶性肿瘤的累积发生率,研究结果发表于近期的《柳叶刀•肿瘤》(The Lancet Oncology)杂志。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#并发#
64
#Lancet#
58
#Oncol#
63
#卵巢肿瘤#
70
#保守治疗#
75
学习了
102