ASCO GI 2015 :MIRO研究:可切除食管癌行混合微创食管切除术有短期获益
2015-01-22 黄蕾蕾 中国医学论坛报
MIRO研究:食管癌患者混合微创和开放性食管切除术比较(摘要号:5) 报告者:Christophe Mariette 报告时间:旧金山时间1月15日,2:00 pm~3:30 pm 研究背景:外科手术被认为是可切除食管癌的唯一治疗选择。术后并发症,特别是肺部并发症,仍然是引起诸多关注的焦点,一半以上行开放性食管切除术(OO)的患者出现并发症。本研究对混合微创食管切除术(HMIO)与OO进行比
MIRO研究:食管癌患者混合微创和开放性食管切除术比较(摘要号:5)
报告者:Christophe Mariette
报告时间:旧金山时间1月15日,2:00 pm~3:30 pm
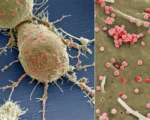
研究背景:外科手术被认为是可切除食管癌的唯一治疗选择。术后并发症,特别是肺部并发症,仍然是引起诸多关注的焦点,一半以上行开放性食管切除术(OO)的患者出现并发症。本研究对混合微创食管切除术(HMIO)与OO进行比较,评价其是否减少并发症的发生。
研究方法:这是一项多中心、非盲、随机对照研究,以2009年10月至2012年4月12家研究中心18~75岁、中段或下1/3段可切除食管癌患者为研究对象,根据计算机生成随机序列分别行经胸廓的OO或HMIO,随机化按研究中心分层。主要研究终点是术后30天Ⅱ~Ⅳ级并发症(手术并发症分级参照Dindo-Clavien分类法)。研究采用意向性分析。
研究结果:共207例患者接受手术,其中OO组104例,HMIO组103例。OO组中有67例(64.4%)患者出现主要术后并发症,HMIO组有37例(35.9%),比值比(OR)为0.31(95%CI:0.18~0.55,P=0.0001)。OO组和HMIO组分别发生主要肺部并发症31例(30.1%)和18例(17.7%)(P=0.037),而术后30天死亡率分别为5例(4.9%)和5例(4.9%)。
研究结论:这一研究结果为可切除食管癌患者行HMIO的短期获益提供证据。
专家点评
主要研究者、法国Claude Huriez大学医院Christophe Mariette:这些结果为HMIO应用于可切除食管癌患者提供了有力的证据。我们认为应该考虑将HIMO作为食管癌手术治疗的一项新的标准方法。
美国Beth Israel Deaconess医学中心、哈佛医学院Michael S. Kent:我认为,微创治疗应该成为这一疾病(可切除食管癌)的标准治疗方案。现在面临的主要挑战是推广如何在其他中心安全开展这项手术,据我所知这是一项有技术要求的手术。另外,手术的操作细节如吻合口的定位、开胸术是否优于胸腔镜等仍未被解决。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#切除术#
65
#ASC#
75
#miR#
87
#食管切除术#
78
#微创#
76
#食管#
68