PLoS One:α-硫辛酸可用于治疗溶栓的缺血性卒中患者
2016-10-31 phylis 译 MedSci原创
背景:α-硫辛酸(aLA)是一种强抗氧化剂,常用于治疗糖尿病多发性神经病。以前,研究表明aLA在大鼠脑缺血后有神经修复效果。然而,其对卒中患者的影响仍然是未知的。研究者调查溶栓治疗的急性缺血性卒中(AIS)给予aLA治疗是否有更好的功能预后。方法:在这项回顾性研究中,172例糖尿病和血浆组织型纤溶酶原激活物(tPA)治疗的AIS患者,研究者调查应用aLA与3个月和1年功能结果的相关性。功能结果包括
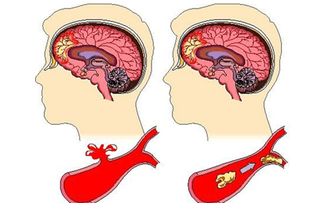
背景:α-硫辛酸(aLA)是一种强抗氧化剂,常用于治疗糖尿病多发性神经病。以前,研究表明aLA在大鼠脑缺血后有神经修复效果。然而,其对卒中患者的影响仍然是未知的。研究者调查溶栓治疗的急性缺血性卒中(AIS)给予aLA治疗是否有更好的功能预后。
方法:在这项回顾性研究中,172例糖尿病和血浆组织型纤溶酶原激活物(tPA)治疗的AIS患者,研究者调查应用aLA与3个月和1年功能结果的相关性。功能结果包括出血性转化(HT),早期神经功能恶化(END),和早期的临床改善(ECI)。良好预后为mRS评分0-2。
结果:在172例AIS和糖尿病患者中,47(27.3%)应用aLA。在整个队列中,应用aLA治疗的患者,3个月和1年的良好预后发生率显著升高。应用aLA治疗的患者,END和HT发生的风险降低,ECI发生的比率增高。在多变量分析中,应用aLA与3个月和1年良好预后相关。年龄,HT,较高的NIHSS分数是良好预后的负性预测因子。
结论:有糖尿病且进行溶栓的AIS患者,应用aLA与预后良好相关。这些结果表明,aLA治疗AIS再灌注治疗后的有效性。
原始出处:
Choi KH, Park MS,et al. Lipoic Acid Use and Functional Outcomes after Thrombolysis in Patients with Acute Ischemic Stroke and Diabetes. PLoS One. 2016 Sep 27
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#缺血性卒中患者#
63
#缺血性卒#
74
#Plos one#
70
#卒中患者#
68
#缺血性#
72