JCEM:血浆雌二醇对绝经早期和晚期妇女亚临床动脉粥样硬化进展的不同影响
2018-10-02 xing.T MedSci原创
由此可见,根据激素治疗开始的时间,E2水平与动脉粥样硬化进展之间的相关性存在差异。随着E2水平的升高,绝经早期女性的CIMT进展率降低,但绝经晚期女性的CIMT进展率则有所上升。这些结果支持HT启动对心血管益处的时间假设,并且在绝经早期开始HT可减缓动脉粥样硬化进展。
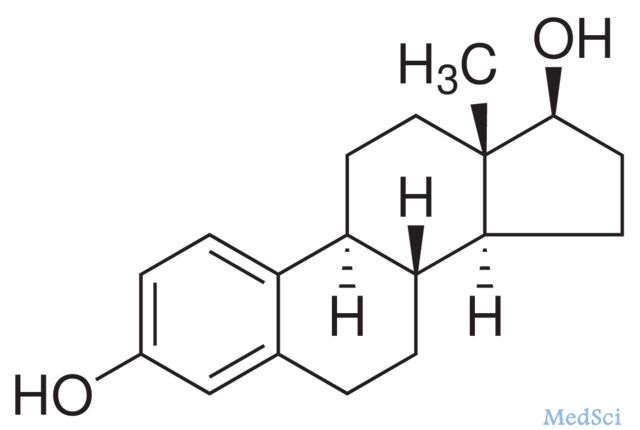
使用雌二醇进行的早期与晚期干预试验表明,在绝经早期而非晚期开始给予激素治疗(HT)可减少动脉粥样硬化的进展。近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究的事后分析旨在确定血浆雌二醇(E2)水平与动脉粥样硬化之间的关系,这种动脉粥样硬化是由颈动脉内膜中层厚度(CIMT)的变化率来决定,并评估了这种关联在绝经早期(<6年)与晚期(≥10年)相比是否同样明显。
因为绝经这一因素,按时间进行分层进行随机对照试验(ClinicalTrials.gov编号为NCT00114517)。研究人员采用混合效应线性模型评估了E2水平与CIMT变化率之间的关联。参与者为健康的绝经后妇女,这些参与者口服E2联合/不联合环状阴道黄体酮。该研究的主要观察指标为平均4.8年期间的血浆E2水平和平均每4个月评估一次的CIMT。
在596名绝经妇女中,较高的E2与绝经早期妇女的CIMT进展呈负相关(p=0.041),而与绝经晚期妇女的CIMT进展呈正相关(p=0.006)(交互作用P<0.001)。绝经早期女性中E2水平的最低与最高四分位数个体CIMT进展率分别为8.5μm/年和7.2μm/年,而绝经晚期女性的CIMT进展率分别为9.8μm/年和11.7μm/年。
由此可见,根据激素治疗开始的时间,E2水平与动脉粥样硬化进展之间的相关性存在差异。随着E2水平的升高,绝经早期女性的CIMT进展率降低,但绝经晚期女性的CIMT进展率则有所上升。这些结果支持HT启动对心血管益处的时间假设,并且在绝经早期开始HT可减缓动脉粥样硬化进展。
原始出处:
Intira Sriprasert,et al. Differential effect of plasma estradiol on subclinical atherosclerosis progression in early versus late postmenopause.J Clin Endocrinol Metab. 2018. https://doi.org/10.1210/jc.2018-01600
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粥样硬化#
103
#JCE#
0
#绝经早期#
47
#亚临床动脉粥样硬化#
67
#JCEM#
65
#绝经#
45
#雌二醇#
93
学习了
151
有用
120
大家一般关心疾病,但是亚临床更重要,这是疾病防控方向的前移,各类疾病都是这样。如亚临床甲减,亚临床心肌损伤,亚临床心衰等
84