Exp Physiol:如何预防胰岛素抵抗与随之而来的糖尿病?
2017-06-24 sunshine2015 来宝网
近期,上海交通大学药学院李大伟教授课题组经过多年研究在肿瘤治疗新靶点研究方面取得重大突破,其研究揭示了乳腺癌中高表达的人前梯度蛋白 2(AGR2)在肿瘤发生发展中的新作用机制。同时,根据相关机制开发的人源化抗体药物 Agtuzumab(18A4Hu)在抗肿瘤及药物联用方面也表现出了优良的治疗效果,相关的一系列研究发表在今年 5 月 8 日的 Nature 子刊《Oncogene》上以及 2016

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言





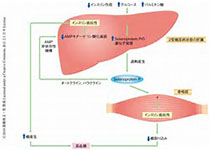






#胰岛#
71
#Physio#
67
非常好的文章,学习了,很受益
116
学习了分享了
92
学习了新知识
111