2019年糖尿病研究进展年终盘点
2020-01-12 MedSci MedSci原创
2019年美国糖尿病协会科学会议于2019年6月7-11日在美国旧金山举行,美国糖尿病年会(ADA年会)是世界上最大、最重要的糖尿病会议,每年都会吸引近18,000名来自世界各地的参与者,其中包括13,000多名医护工作人员等。5天的会议,为与会者提供与领先的糖尿病专家交流互动、分享看法,为研究人员和医疗保健专业人士提供了解当前关于糖尿病研究、治疗和护理的重大进展,以及访问超过
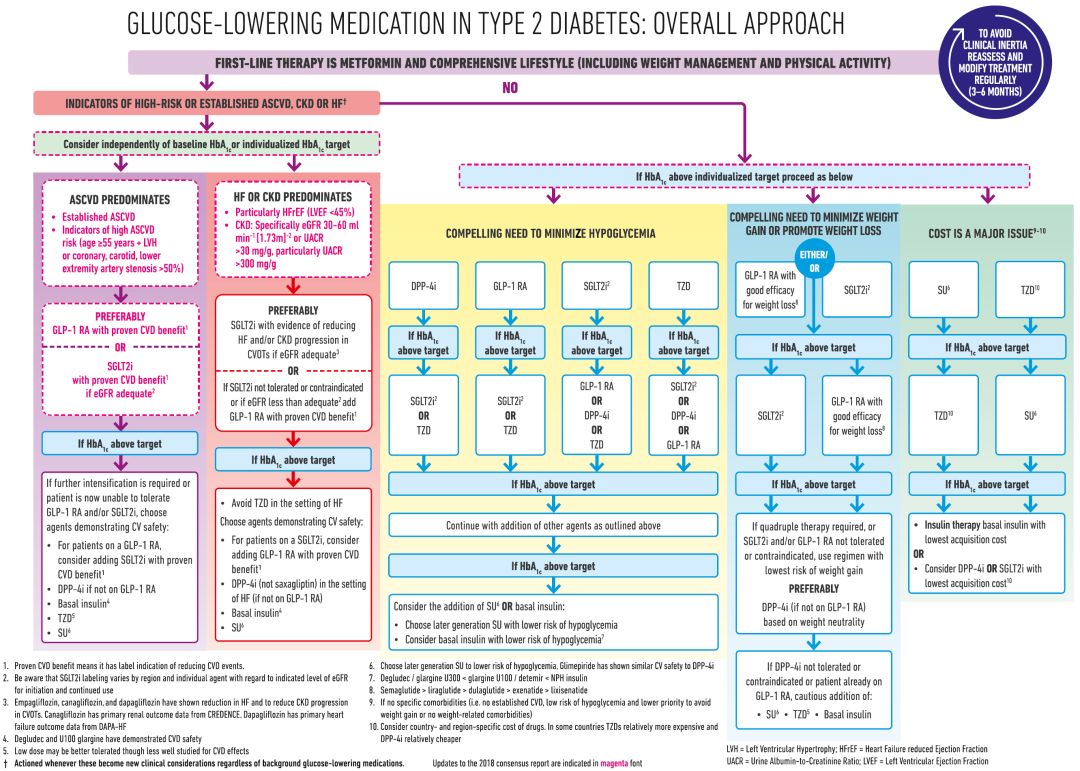
《2020年ADA糖尿病医学诊疗标准》公布 “是否应将成年人缓慢进展的自身免疫性糖尿病称为成人隐匿型自身免疫性糖尿病”的争论已有定论 ➤ 增加了一项新的关于超重或肥胖和/或伴有一个或多个额外糖尿病危险因素并计划妊娠的女性糖尿病前期和/或2型糖尿病的检测推荐(2.8)。 ➤ 在“囊性纤维化相关糖尿病”(CFRD)部分增加了使用糖化血红蛋白(A1C)检测CFRD的注意事项。 ➤ 新增“胰腺性糖尿病或外分泌腺胰疾病背景下的糖尿病”章节,描述了该类型的糖尿病及其多种病因。 ➤ 修订了“妊娠期糖尿病”(GDM)部分,筛查与诊断GDM的两步法不再包括国家糖尿病数据组标准。ADA/EASD最新共识 对于伴有致动脉粥样硬化性心血管疾病(如伴有心肌梗死、缺血性卒中、有ECG改变的不稳定心绞痛、影像学检查或负荷试验显示的心肌缺血、冠脉/颈动脉/外周动脉血运重建)的T2DM患者,MACE是最严重的威胁。这些患者应用GLP-1受体激动剂实现MACE获益的证据最强。 基于REWIND研究最新结果推荐,无心血管疾病但存在相关高危因素(尤其是年龄≥55岁伴有冠脉/颈动脉/下肢
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#研究进展#
77
#年终盘点#
92
好好好好好好
125
学习了
117
谢谢MedSci提供最新的资讯
108
***
113