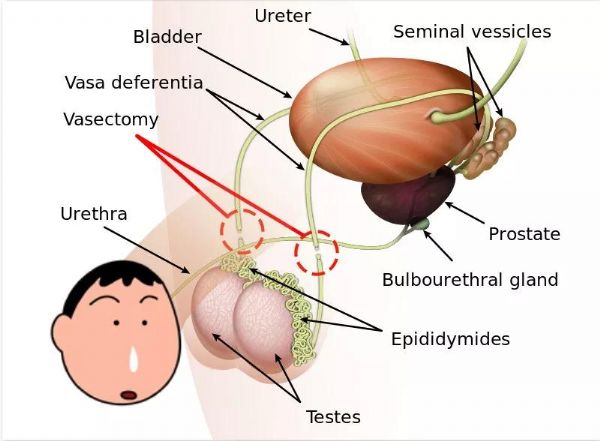
J Natl Cancer Inst:男默女泪!215万男性随访38年发现,输精管结扎与前列腺癌风险增加15%有关
2019-05-31 奇点糕 奇点网
出于各种原因,男性结扎相对来说一直是个比较禁忌的话题,大家对它的了解也并不多。每当看到有人问“结扎之后是不是就不能做爱做的事了”的时候,奇点糕就觉得莫名好笑,你们对结扎到底是有什么误解啊?

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
55
#前列腺癌风险#
0
#ATL#
68
#输精管#
67
#癌风险#
56
#NST#
42
前列腺癌相关研究,学习了,谢谢梅斯
74
学习了,谢谢分享
76