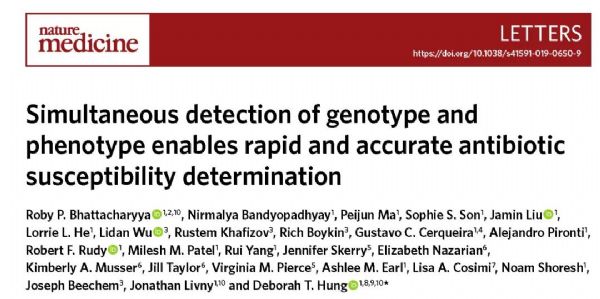
Nat Med:同时检测基因型和表型,新方法稳准快检测抗生素敏感性!
2019-12-02 Eagle 转化医学网
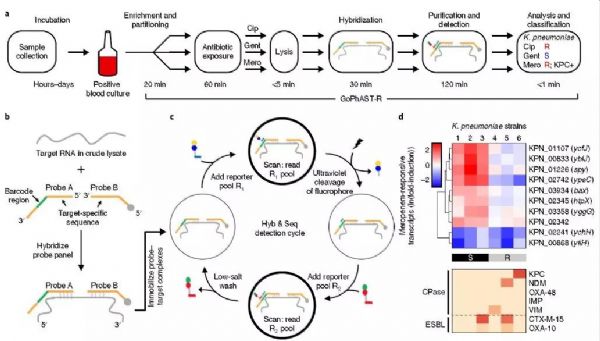
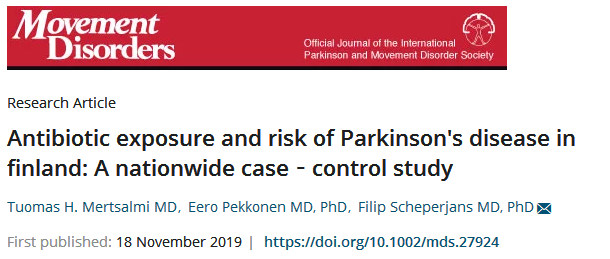
抗生素与我们的生活密切相关,它就像一把“双刃剑”,昔日是对抗疾病延长生命的“万能神药”,随着高频率滥用,而今抗生素的耐药性问题已成为世界卫生领域的重大难题,并严重威胁人类健康。由此,在临床治疗中,快速检测抗生素敏感性技术将为人类带来新福音。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#新方法#
55
#Nat#
56
#基因型#
0
#敏感性#
55
#表型#
53
#Med#
50