Neurology:非交叉性视网膜纤维综合征(无视交叉综合征)
2018-06-15 zyx整理 神经科病例撷英拾粹
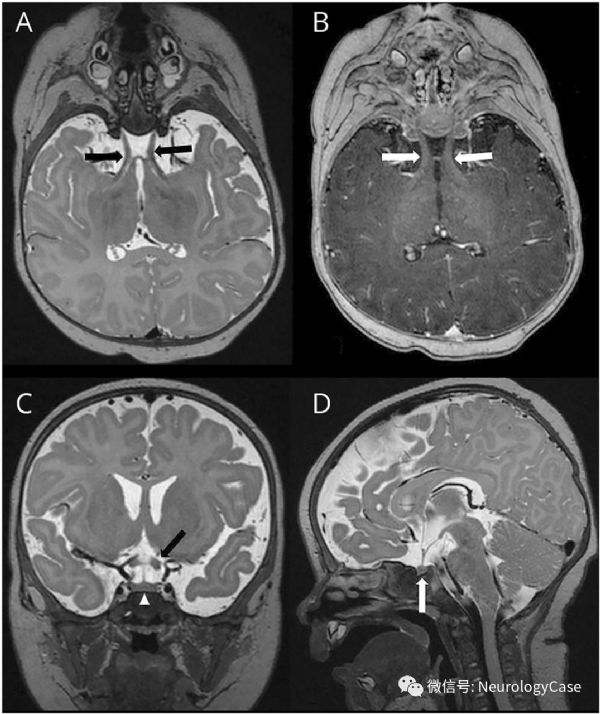
9周女婴,表现为视觉刺激反应差和先天性跷跷板眼球震颤(seesaw nystagmus)。先天性跷跷板眼球震颤通常提示结构性异常,如无视交叉,需行MRI明确(图)
9周女婴,表现为视觉刺激反应差和先天性跷跷板眼球震颤(seesaw nystagmus)。先天性跷跷板眼球震颤通常提示结构性异常,如无视交叉,需行MRI明确(图)。孤立的视交叉缺如是非常罕见的。在非交叉性视网膜纤维综合征(nondecussating retinal-fugal fiber syndrome)(无视交叉综合征[achiasmatic syndrome])中,鼻侧的视网膜纤维交叉失败,误传的鼻侧纤维投射扰乱了同一眼颞侧视网膜纤维的投射,导致左右半部分视野坐标反转(“镜像反转”)。 同源框基因突变可能是视网膜轴突发育过程中出现这种无交叉变异的基础。
(图:A-B:视神经水平T2WI和增强T1可见视神经纤维在延续成为视束前未能形成交叉结构[黑箭和白箭],为无视交叉综合征的特点;C-D:鞍区水平冠状位和矢状位T2WI证实视交叉缺如[黑箭:视束;白箭头和箭:垂体])
原始出处:
Nikam R, Kandula V, Donuru A. Nondecussating retinal-fugal fiber syndrome (achiasmatic syndrome).Neurology. 2018 May 22;90(21):979-980.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Neurol#
115
#视网膜#
112
#综合征#
101
谢谢分享.学习了
133
学习了.长知识
126