心衰和室性心律失常,互为因果的难兄难弟!
2018-03-21 佚名 医学界心血管频道
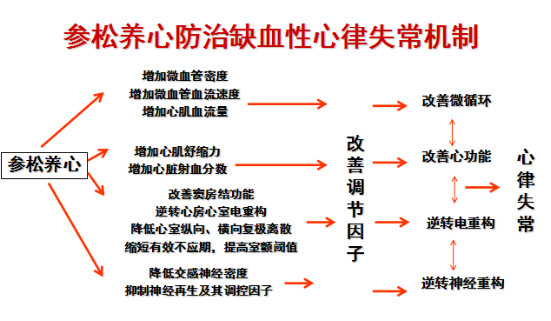
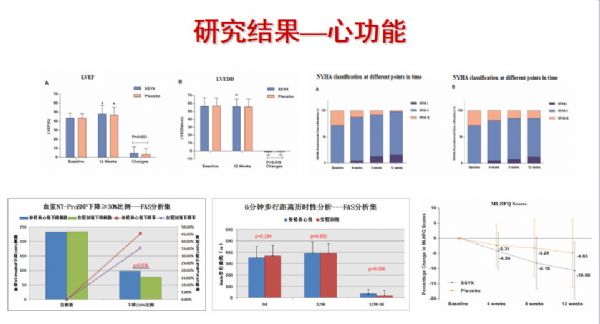
3月17日,第十四届国际络病学大会在泉城济南隆重召开。武汉大学人民医院黄从新教授带来了以《心衰合并室性心律失常的治疗》为题的精彩报告,重点讲解了心衰合并室性心律失常的管理原则与治疗方法,并介绍了参松养心用于治疗心衰合并室性心律失常的相关研究。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











好
110
学习了
0
好
109
好文.值得点赞.更值得收藏!慢慢领会学习的.给点个赞!
0
学习了
113
学习了
61
谢谢分享学习
66