BMC Musculoskelet Disord:控制远端锁定螺钉与胫距关节切线的夹角有助于减少髓内钉内固定治疗的胫骨远端骨折错位的发生
2022-09-15 医路坦克 MedSci原创
本文探讨了胫骨远端带锁螺钉与胫距关节切线(ADTTS)在矢状面和冠状面形成的角度与IMN内固定治疗胫骨远端骨折术后对位的关系。
背景:研究表明,在冠状面上,远端锁定螺钉的方向是否与胫距关节切线平行,可以判断髓内钉内固定治疗胫骨远端骨折后有无内翻或外翻畸形。然而,目前还没有关于冠状面夹角的统计分析,也没有关于远端锁定螺钉在矢状面上的方向或胫距关节切线夹角与胫骨远端骨折髓内钉内固定术后对位关系的报道。
目的:探讨胫骨远端带锁螺钉与胫距关节切线(ADTTS)在矢状面和冠状面形成的角度与IMN内固定治疗胫骨远端骨折术后对位的关系。
方法:对100例胫骨远端骨折患者进行回顾性分析,其中100例患者采用经膝上入路IMN内固定治疗。在冠状面和矢状面上,ADT由小到大分为A、B、C、D 4组,用单因素方差分析比较各组间胫骨远端外侧角(LDTA)和胫骨前远角(ADTA),用卡方检验比较各组间术后胫骨错位的发生率。采用卡方检验确定可能与脱位相关的因素,包括腓骨切开复位内固定(ORIF)、有限切开复位、ADTT、IMN直径、损伤机制、开放性骨折与闭合性骨折、粉碎性骨折和腓骨骨折平面。然后,将单变量分析中具有统计学意义的变量纳入多变量Logistic回归方程,以评估与错位相关的独立因素。

图1 ADTT的测量
在冠状平面上,测量带锁髓内钉远端投影线与胫距关节切线之间的ADTT。当指向内侧时,角度为负。在矢状面上,测量带锁螺钉远端前后方向投影线与胫距关节切线之间的ADTT。当指向前方时,角度为正
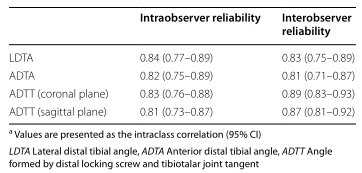
表1 所有DR测量的观察员间和观察员内可靠性


图2 矢状面:A组和D组与B组和C组对齐不良的显著差异
结果:在冠状平面上,A、B、C、D组的ADT分别为<0°、0°~1.3°、1.3°~2.7°和>2.7°。B组和C组(0°~1.3°和1.3°~2.7°)、A组(<0°)和D组(>2.7°)的平均LDTA分别为89.5±1.6°、92.0±3.2°和85.8±3.5°(P<0.01)。畸形>5°者,A、D组多于B、C组[14/50(28%)vs 1/50(2%),P<0.001]。在矢状面上,A、B、C、D组ADTT值分别为<8.9°、8.9°~10.4°、10.4°~11.7°和>11.8°。B、C组(8.9°~10.4°和10.4°~11.7°)、A组(<8.9°)和D组(>11.8°)平均ADTA分别为80.4±1.3°、83.1±3.7°和77.9±2.5°(P<0.01)。畸形>5°者,A、D组多于B、C组[13/50(26%)vs 0/50(0%),P<0.001]。冠状面ADTT为0°~2.7°,矢状面为8.9°~11.7°(OR:0.08,P=0.02)和有限切开复位(OR:0.21,P<0.01)是减少错位的独立因素。
结论:胫骨远端骨折术后对ADTT和有限切开复位的选择较为敏感。控制ADTT在冠状面0°~2.7°和矢状面8.9°~11.7°之间有利于减少IMN内固定治疗胫骨远端骨折后对位错位的发生。
文献来源:
He M, Liu J, Deng X,Controlling the angle between the distal locking screw and tibiotalar joint tangent helps to reduce the occurrence of misalignment of distal tibial fractures treated with intramedullary nail fixation.BMC Musculoskelet Disord 2022 Jul 14;23(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#BMC#
103
#Dis#
63
#Disord#
57
#胫骨#
0
#髓内钉#
57
#内固定#
56