JAMA Network Open:临床决策支持工具可降低严重精神疾病患者心血管病风险
2022-03-17 影像小生 MedSci原创
CDS 干预可实现干预患者总可改变 CV 风险的变化率比对照患者低 4%
患有双相情感障碍、精神分裂症或分裂情感性障碍的人,统称为严重精神疾病(SMI),其死亡率是无SMI人群的2.3倍,寿命缩短10至15年。心血管(CV)疾病是重度精神病患者的主要死亡原因,与血脂异常(5倍)、吸烟(2倍至3倍)、糖尿病(2倍)和肥胖(1.5倍至2倍)的较高相对风险有关。一些SMI药物可能通过对体重、胰岛素抵抗和脂质代谢产生不利影响而增加心脏代谢风险。理论上,通过早期识别和管理可改变的CV危险因素以及其他策略,可以降低重度精神分裂症患者的CV超额死亡率。
临床决策支持(CDS)工具通常是基于技术的干预措施,通常在护理点提供针对患者的信息,以改善健康和保健初级保健环境中的临床决策支持可以帮助临床医生解决循证护理方面的空白,但许多以前的CDS研究都没有结果,部分原因是CDS设计不佳和CDS工具使用率低。随着设计和实施的改进,更多与电子健康记录(EHR)相关的CDS工具的最新研究已经实现了高使用率,并降低了没有SMI群的CV风险。
Rebecca C. Rossom等在JAMA Network Open杂志发表题为Effect of Clinical Decision Support on Cardiovascular Risk Among Adults With Bipolar Disorder, Schizoaffective Disorder, or Schizophrenia A Cluster Randomized Clinical Trial的研究文章,评估针对初级保健临床医生的临床决策支持 (CDS) 系统是否能改善成年初级保健 SMI 患者的心血管健康。
在 2016 年 3 月 2 日至 2018 年 9 月 19 日进行的这项整群随机临床试验中,限制性随机化分配了 3 个中西部医疗保健系统的 76 家初级保健诊所接受或不接受旨在改善 CV 的 CDS 系统SMI 患者的健康状况。符合条件的诊所至少有 20 名 SMI 患者;临床医生及其成年 SMI 患者至少有 1 个可改变的 CV 风险因素未达到美国心脏病学会/美国心脏协会指南设定的目标。
从 2019 年 1 月 10 日到 2021 年 12 月 29 日,在意向治疗的基础上进行了统计分析。采用CDS 系统评估了可改变的 CV 风险因素,并为临床医生和患者提供了个性化的治疗建议。个体可改变的风险因素(吸烟、体重指数、低密度脂蛋白胆固醇水平、收缩压和血红蛋白 A1c 水平)相加得到12 个月内总可改变 CV 风险的变化。
该研究共纳入 8937 名 SMI 患者(4922 名女性 [55.1%];平均 [SD] 年龄,48.4 [13.5] 岁)。
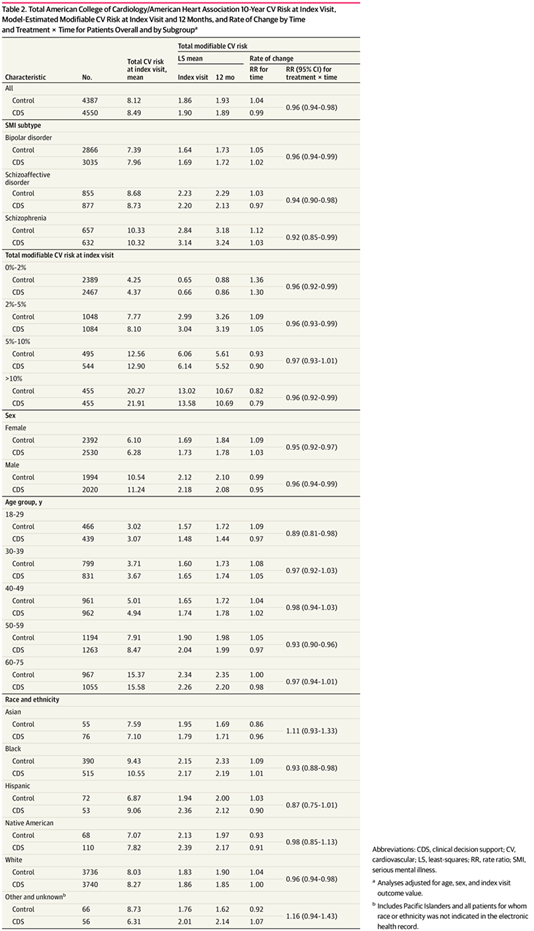
相对于对照患者,干预患者的总可改变 CV 风险增加率降低了 4%(相对比率 [RR],0.96;95% CI,0.94-0.98)。
干预有利于 18 至 29 岁(RR,0.89;95% CI,0.81-0.98)或 50 至 59 岁(RR,0.93;95% CI,0.90-0.96)、黑人(RR, 0.93;95% CI,0.88-0.98)或白色(RR,0.96;95% CI,0.94-0.98)。
男性(RR,0.96;95% CI,0.94-0.99)和女性(RR,0.95;95% CI,0.92-0.97),以及任何 SMI 亚型(双相情感障碍:RR,0.96;95% CI, 0.94-0.99;分裂情感障碍:RR,0.94;95% CI,0.90-0.98;精神分裂症:RR,0.92;95% CI,0.85-0.99)也从干预中受益。
尽管治疗效果有利于干预,但个体可改变的风险因素没有显着差异。
这种 CDS 干预可实现干预患者总可改变 CV 风险的变化率比对照患者低 4%。结果是由个体可修改风险因素的增量和大多数不显着变化的累积效应驱动的。这些发现强调了使用 CDS 促进成人 SMI 早期初级保健干预的价值。
原文出处
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#NET#
87
#临床决策#
85
#血管病#
69
#PE#
59
#疾病患者#
67
#严重精神疾病#
60
#决策#
66